Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (15 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
13.81Mb size Format: txt, pdf, ePub
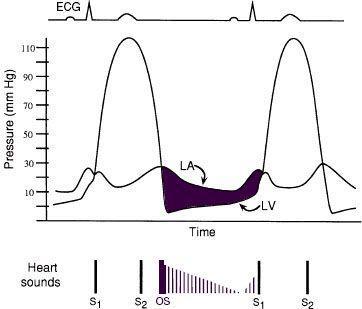
MVA proportional to S
2
–OS interval (tighter
valve → ↑ LA pressure → shorter interval)
• Loud S
1
(unless MV calcified)
Diagnostic studies
• ECG:
LAE
(“P mitrale”), ± AF, ± RVH
• CXR:
dilated LA
(straightening of left heart border, double density on right, left mainstem bronchus elevation) •
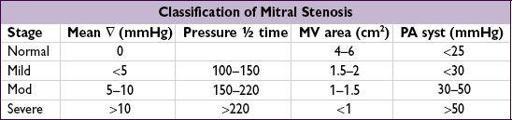
Echo
: estimate pressure gradient (∇), RVSP, valve area, valve echo score (0–16, based on leaflet mobility & thick., subvalvular thick., Ca
++
); exer. TTE (to assess ∆ RVSP and ∇) if sx & severity of MS at rest discrepant; TEE to assess for LA thrombus before PMV
•
Cardiac cath
: ∇ from simultaneous PCWP & LV pressures, calculated MVA; LA pressure tall
a
wave and blunted
y
descent; ↑ PA pressures
Treatment (
NEJM
1994;331:961;
Circ
2002;105:1465 & 2008;118:e523;
EHJ
2012;33:2451)
• Medical: Na restriction, cautious diuresis, bB, sx-limited physical stress • Antibiotic Ppx recommended if h/o RHD w/ valvular disease for 10 y or until age 40
• Anticoag if: AF, prior embolism, LA thrombus; ? LA >55 mm or lg LA w/ spont contrast • Mechanical intervention if: heart failure sx w/ MVA ≤1.5, or
heart failure sx w/ MVA >1.5 but ↑ PASP, PCWP, or MV ∇ w/ exercise, or
asx Pts w/ MVA ≤1.5 and PHT (PASP >50 or >60 mmHg w/ exercise) or new-onset AF
•
Percutaneous mitral valvotomy
(PMV): preferred Rx if RHD; MVA doubles, ∇↓ by 50%;MVR
if
valve score <8, ≤ mild MR, AF or LA clot • Surgical (MV repair if possible, o/w replacement): consider in sx Pts w/ MVA ≤1.5
if PMV unavailable/contraindicated (mod. MR, LA clot), or valve morphology unsuitable
• Pregnancy: if NYHA class III/IV → PMV, o/w medical Rx w/ low-dose diuretic & bB
MITRAL VALVE PROLAPSE (MVP)
Definition and Etiology
• Billowing of MV leaflet ≥2 mm above mitral annulus in parasternal long axis echo view • Leaflet redundancy from myxomatous proliferation of spongiosa of MV apparatus • Idiopathic, familial and a/w connective tissue diseases (eg, Marfan’s, Ehlers-Danlos) • Prevalence 1–2.5% of gen. population,>
(
NEJM
1999;341:1), most common cause of MR
Clinical manifestations (usually asymptomatic)
• MR (from leaflet prolapse or ruptured chordae); infective endocarditis; embolic events • Arrhythmias, rarely sudden cardiac death
Physical exam
• High-pitched, midsystolic click ± mid-to-late systolic murmur
• ↓ LV volume (standing) → click earlier; ↑ LV volume or afterload → click later, softer
Treatment
• Endocarditis prophylaxis no longer recommended (
Circ
2007:116:1736) • Aspirin or anticoagulation if prior neurologic event or atrial fibrillation
TRICUSPID REGURGITATION
• Primary etiol: rheumatic, CTD, radiation, IE, Ebstein’s anomaly, carcinoid, tumors
• Fxnal etiol: RV and/or pulm HTN (may be 2° to L-sided dis.), RV dilation and/or infarct
• Consider repair, annuoplasty or replacement for sx and severe TR (eg, ERO ≥0.40 cm
2
)
PROSTHETIC HEART VALVES
Mechanical (60%)
•
Bileaflet
(eg, St. Jude Medical); tilting disk; caged-ball • Very durable (20–30 y), but thrombogenic and ∴ require anticoagulation
consider if age <~65 y or if anticoagulation already indicated (
JACC
2010;55:2413)
Bioprosthetic (40%)
• Bovine
pericardial
or porcine
heterograft
(eg, Carpentier-Edwards), homograft • Less durable, but min. thrombogenic; consider if >~65 y, lifespan <20 y or anticoag
Physical exam
• Normal:
crisp sounds
, ± soft murmur during forward flow (normal to have small ∇) • Abnormal: regurgitant murmurs, absent mechanical valve closure sounds
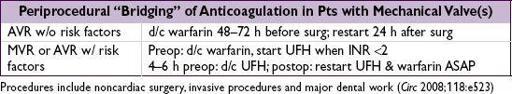
Anticoagulation & antiplatelet therapy (
Circ
2008;118:e523;
JAMA
2012;308:2118)
• Assess for
high-risk features
: prior thromboembolism, AF, EF<30–35%, hypercoagulable •
Warfarin
: low-risk mech AVR: INR 2–3 (consider 2.5–3.5 for 1st 3 mo)
mech MVR or high-risk mech AVR: INR 2.5–3.5
high-risk bioprosthetic: INR 2–3 (and consider in low-risk for 1st 3 or even ? 6 mo)
•
ASA
(75–100 mg) for all prosthetic valves; avoid adding to warfarin if h/o GIB, uncontrolled HTN, erratic INR or >80 y;
ASA
+
clopidogrel
(or warfarin) × 3–6 mo after TAVR
• If thrombosis, ↑ intensity (eg, INR 2–3 → 2.5–3.5; 2.5–3.5 → 3.5–4.5; add ASA if not on)
Correction of overanticoagulation (
Circ
2008;118:e626)
• Risk from major bleeding must be weighed against risk of valve thrombosis • Not bleeding: withhold warfarin, give vit K 1–2.5 mg
PO
only if INR 5–10, ✓ serial INRs • Bleeding or INR >10: FFP ± low-dose (1 mg) vit K IV
Endocarditis prophylaxis: for all prosthetic valves (see “Endocarditis”)
Complications
• Structural failure (r/o endocarditis); mechanical valves: rare except for Bjork-Shiley; bioprosthetic valves: up to 30% fail rate w/in 10–15 y, mitral > aortic • Paravalvular leak (r/o endocarditis); small
central
jet of regurg is normal in mech. valves • Obstruction from thrombosis or pannus ingrowth: ✓ TTE, TEE and/or fluoroscopy if ? clot significantly sx
pannus
ingrowth: remove w/ surgery
thrombosis: surgery if L-sided valve & either severe sx or lg (? >1 cm) clot burden; lytic often
ineffective
for L-sided thrombosis & 12–15% risk of stroke; consider UFH ± lytic (? low-dose tPA via slow infusion,
JACC CV Imaging
2013;6:206) if mild sx & small clot burden or poor surg candidate; lytic reasonable for R-sided
• Infective endocarditis ± valvular abscess and conduction system dis. (see “Endocarditis”) • Embolization (r/o endocarditis); risk ~1%/y w/ warfarin (vs. 2% w/ ASA, or 4% w/o meds)
mech MVR 2 × risk of embolic events vs. mech AVR (
Circ
1994;89:635)
• Bleeding (from anticoag), hemolysis (esp. w/ caged-ball valves or paravalvular leak)
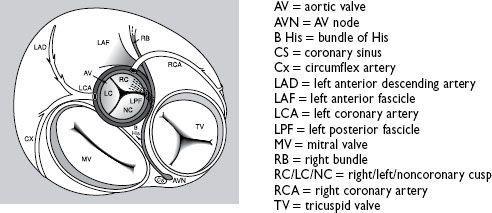
HEART VALVES (superior view,
JAMA
1976;235:1603)
Other books
The Undoing of de Luca by Kate Hewitt
Diary of a Chav by Grace Dent
The 8th Circle by Sarah Cain
El maestro iluminador by Brenda Rickman Vantrease
America's White Table by Margot Theis Raven, Mike Benny
Their Virgin Mate [Panther Cove 5] (Siren Publishing Ménage Everlasting) by Melody Snow Monroe
The Strongest Steel by Scarlett Cole
Desires' Guardian by Tempeste O'Riley
The Mamur Zapt and the Spoils of Egypt by Michael Pearce
Glamour of the God-Touched by Ron Collins