Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (71 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.62Mb size Format: txt, pdf, ePub
• CR achieved in 70–80% of Pts <60 y and in 40–50% for Pts >60 y • Overall survival depends on prognostic factors: ranges from ~50% for Pts <60 y w/ favorable prognostic factors to <10% for Pts >60 y w/ poor prognostic factors • Poor prognostic factors:
age
>
60
, unfavorable cytogenetics (see above), FLT3-ITD, poor performance score, antecedent MDS/MPN, therapy-related AML; genetic profiling (
NEJM
2012;366:1079)
Acute promyelocytic leukemia (APL)
(
Blood
2009;113:1875)
• Rare disease w/ only ~1000 cases/y in the U.S.
but biologically and clinically distinct
• Atypical promyelocytes (large, granular cells; bilobed nuclei) in blood and bone marrow • Defined by translocation of retinoic acid receptor:
t(15;17)
;
PML-RAR
ɑ
(>95% of cases) •
Medical emergency
with
DIC
and
bleeding
common; supportive care measures crucial • Remarkable responses to
all-
trans
-retinoic acid (ATRA)
, which induces differentiation, and
arsenic trioxide (ATO)
; early initiation of ATRA is critical as soon as APL
suspected
; ATO highly active as first-line therapy or in treatment of refractory disease.
• Induction regimen: anthracycline + ATRA ± cytarabine → CR in ~90%; or ATRA + ATO alone (ASH 2012;
JCO
2009;27:504) • Differentiation (ATRA) syndrome: ~25% of Pts; fever, pulm infiltrates, SOB, edema, HoTN, AKI; tx w/ dexamethasone 10 mg bid, supportive care (eg, diuresis) (
Blood
2008;113:775) • Consolidation Rx: eg, ATO → anthracycline + ATRA (
Blood
2010;116:3751) • Role of maintenance Rx (eg, ATRA + 6MP + MTX) currently controversial • Best prognosis of all AMLs: >90% cure; WBC >10,000/µL = ↓ prognosis (
Blood
2000;96:1247)
ACUTE LYMPHOBLASTIC LEUKEMIA (ALL)
Classification
• Lymphoblastic neoplasms may present as acute leukemia (ALL) with
>20% BM blasts
or as lymphoblastic lymphoma (LBL) w/ mass lesion & <20% BM blasts. ALL and LBL are considered the same disease with different clinical presentations.
• Morphology:
no granules
(granules seen in myeloid lineage) • Cytochemistry:terminal deoxynucleotidyl transferase (TdT) in 95% of ALL
• Cytogenetics (
Blood
2010;115:206): t(9;22) = Philadelphia chrom (Ph) ~25% of adults w/ ALL
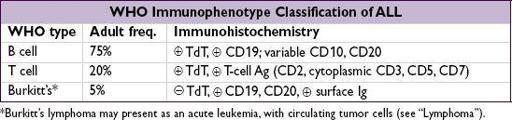
• Immunohistochemistry: 3 major phenotypes (Burkitt’s usually treated differently)
Treatment
(
NEJM
2006;354:166;
JCO
2011;29:532)
•
Induction chemo
: multiple acceptable regimens including combination of anthracycline, vincristine, steroids, cyclophosphamide, ± asparaginase •
CNS prophylaxis
: intrathecal MTX/cytarabine ± cranial irradiation
or
systemic MTX
•
Postremission therapy
options:
consolidation/intensification chemo (~7 mo) followed by maintenance chemo (~2–3 y) high-dose chemo w/ allo HSCT considered for all Pts in CR1 w/ available donor pediatric regimens in young adults (<30 y); consider allo SCT for all Pts <50 (controversial)
• If relapse → salvage chemo followed by allogeneic HSCT if able • Pht(9;22) → add imatinib or dasatinib, followed by allogeneic HSCT
• MLL-AF4 t(4;11) or hypodiploidy (<44 chromosomes) → consider for allogeneic HSCT
• Infusion of chimeric antigen receptor–modified T cells promising (
NEJM
2013;368:1509)
Prognosis
• CR achieved in >80% of adults
• Cure achieved in 50–60% if good prog. factors vs. 10–30% w/ poor prog. factors • Good prognostic factors: younger age, WBC <30,000/µL, T-cell immunophenotype, absence of Ph chromosome or t(4;11), early attainment of CR
• Gene expression patterns may be useful in predicting chemo resistance (
NEJM
2004;351:533)
CHRONIC MYELOGENOUS LEUKEMIA (CML)
Definition
(
Blood
2009;114:937)
•
Myeloproliferative neoplasm
with clonal overproduction of hematopoietic myeloid stem cells that can differentiate •
Philadelphia chromosome
(Ph) = t(9;22) →
BCR-ABL
fusion → ↑ Abl kinase activity
BCR-ABL
required for Dx of CML
• “Atypical CML” (BCR-ABL) now considered a separate disease and reclassified as MDS/MPN (see “Myelodysplastic Syndromes”)
Epidemiology and risk factors
•
5400 new cases/y in U.S.; median age
64 at presentation; ~15% of adult leukemias • ↑ risk with irradiation; no clear relation to cytotoxic drugs
Clinical manifestations
• Triphasic clinical course; 85% present in the chronic phase •
Chronic phase
: often asymptomatic but common features are fatigue, malaise, weight loss, night sweats, abdominal fullness (
splenomegaly
50%) •
Accelerated phase
: refractory leukocytosis, thrombocytopenia and worsening sx → fever, wt loss, ↑ splenomegaly, bone pain, bleeding, infections, pruritus (basophilia) •
Blastic phaseacute leukemia → severe constitutional symptoms, infection, bleeding and possible
leukostasis
(see “Acute Leukemia”)
Diagnostic evaluation
•
Peripheral smear
:
leukocytosis
(often >100,000/µL), left-shifted with
all stages of
myeloid maturation
; anemia, thrombocytosis,
basophilia
•
Bone marrow
: hypercellular, ↑ myeloid to erythroid ratio, ↓ leuk alkaline phosphatase •
Chronic
: <10% blasts (peripheral or BM) •
Accelerated
: 10–20% blasts, >20% basos, plts <100k, ↑ spleen size, karyotypic prog.
•
Blastic
: >20% blasts (
2
⁄
3
myeloid,
1
⁄
3
lymphoid), may see extramedullary leukemia
Treatment
(
NEJM
2010;362:2260;
Blood
2011;118:1208 & 2012;120:1390)
•
Tyrosine kinase inhibitor (TKI)
: imatinib, dasatinib, nilotinib, bosutinib, ponatinib are selective inhibitors of BCR-ABL (
JCO
2010;28:428;
Blood
2012;120:1390).
Imatinib, nilotinib, & dasatinib approved as initial Rx.
Resistance = recurrent dis. on TKI, often result of
BCR-ABL
mutation or amplification.
Nilotinib, dasatinib, bosutinib, & ponatinib approved for resistant disease, w/ only ponatinib effective on T315I resistance mutation (
NEJM
2012;367:2075).
Side effects include nausea, diarrhea, muscle cramps, cytopenias, ↓ PO
4
, ↑ QT, rarely CHF; dasatinib also a/w pericardial & pleural effusions, nilotinib w/ ↑ bili & lipase.
•
Chronic phase
: TKI; continued indefinitely in responders (
Blood
2012;120:1390) •
Accelerated phase
: TKI upfront, consider allogeneic HSCT
Other books
Ostrich: A Novel by Matt Greene
Long Gone Man by Phyllis Smallman
The Girl Before by Rena Olsen
What the Nose Knows: The Science of Scent in Everyday Life by Avery Gilbert
Shifting Gears by Jenny Hayut
STARGATE SG-1: Do No Harm by Karen Miller
Dominion: Zoë Martinique Investigation, Book 6 by Phaedra Weldon
The Meq by Steve Cash
Rumpole and the Penge Bungalow Murders by John Mortimer
Gawky by Margot Leitman