Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (72 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
13.55Mb size Format: txt, pdf, ePub
•
Blastic phase
: TKI + HSCT vs. ALL or AML induction (based on cell type) + HSCT
•
Allogeneic HSCT
: consider for Pts w/ available donor who present in accelerated or blastic phase; reasonable option for Pts with relapsed/refractory disease to TKIs
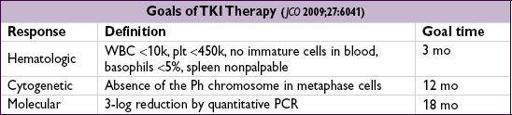
Prognosis
• Chronic phase CML Rx’d w/ imatinib: 89% overall survival, 95% survival free of CML-related deaths, 7% progression to blast phase at 5 y (
NEJM
2006;355:2408) • Accelerated phase CML Rx’d w/ imatinib: ~50% overall survival at 4 y (
Cancer
2005;103:2099) • Poor prognostic factors: ↑ age, ↑ platelet count, ↑ spleen size, ↑ percentage of blasts
CHRONIC LYMPHOCYTIC LEUKEMIA (CLL)
Definition
(
NEJM
2005;352:804;
Blood
2008;111:5446)
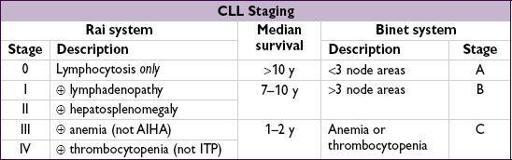
• Monoclonal accumulation of functionally incompetent mature B lymphocytes • CLL (>5000/µL malignant cells) & small lymphocytic lymphoma (SLL; <5000/µL malignant cells, but + LAN ± splenomegaly) now classified as same disease • Monoclonal B lymphocytosis (<5000/µL, nodes <1.5 cm, nl RBC and Plt counts): observe
Epidemiology and risk factors
• ~16,000 new cases/y; median age at dx is 72 y; most common adult leukemia • ↑ incidence in 1st-degree relatives; no known association with radiation, chemicals, drugs
Clinical manifestations
• Symptoms:
often asx
& identified when CBC reveals lymphocytosis; 10–20% p/w fatigue, malaise, night sweats, weight loss (ie, lymphoma “B” sx) • Signs:
lymphadenopathy
(80%) and
hepatosplenomegaly
(50%) •
Autoimmune hemolytic anemia
(AIHA) (~7%) or
thrombocytopenia
(ITP) (~1–2%) • Hypogammaglobulinemia ± neutropenia → ↑ susceptibility to
infections
• Bone marrow failure in
13%; monoclonal gammopathy in
5%
• Aggressive transformation: ~5% develop
Richter’s syndrome
= transformation into high-grade lymphoma (usually DLBCL) and sudden clinical deterioration
Diagnostic evaluation
(see “Lymphoma” for general approach)
•
Peripheral smear
:
lymphocytosis
(>5000/µL, mature-appearing small cells) “
smudge
” cells from damage to abnl lymphs from shear stress of making blood smear •
Flow cytometry
:
clonality
with dim surface Ig (sIg); CD5+, CD19+, CD20(dim), CD23+. CD38+ or ZAP70+ a/w unmutated Ig variable heavy chain region & worse prognosis.
•
Bone marrow
: normo-or hypercellular; infiltrated w/ small B-cell lymphocytes (≥30%) •
Lymph nodes
: infiltrated w/ small lymphocytic or diffuse small cleaved cells = SLL
•
Genetics
: del 11q22-23 & 17p13 unfavorable; trisomy 12 neutral; del 13q14 and mut
IgVH
favorable. Nine significantly mutated genes, including
TP53
,
NOTCH1
,
MYD88
and
SF3B1
. Key role for spliceosome mutations (
NEJM
2011;365:2497;
JCI
2012;122:3432).
Treatment
• Treatment is primarily
palliative
→ early stage disease can be followed w/o Rx • Indications for treatment: Rai stages III/IV, Binet stage C, disease-related sx, progressive disease, AIHA or ITP refractory to steroids, recurrent infections • Options:
purine analogues
: fludarabine (“F”), pentostatin (“P”)
alkylating agents
: cyclophosphamide (“C”), bendamustine (“B”), CVP, CHOP; ? chlorambucil for elderly (lower response vs. F, butsurvival;
NEJM
2000;343:1750)
±
monoclonal Ab
against CD20 (
rituximab
, “R”) or CD52 (alemtuzumab, esp. w/ 17p-)
combination regimens
(eg, FR, FCR, BR) superior to monoRx (
Lancet
2007;370:230)
• Novel Rx refractory dis.: ofatumumab (ɑ-CD20), ibrutinib (BTK inhib), CAL101 (PI3K inhib) • Consider allo-HSCT in
p53
mut or refractory CLL (
BBMT
2009;15:53;
BJH
2012;158:174) • Supportive care: PCP, HSV, VZV prophylaxis; CMV monitoring for Pts receiving anti-CD52; AIHA/ITP → steroids; recurrent infections → IVIg
Prognosis
(
NEJM
2004;351:893;
JCO
2006;24:4634 & 2010;28:4473;
Blood
2008;111:865)
• Survival varies substantially. Median overall survival ~10 y (
Am J Hematol
2011;12:985) • Favorable prognosis: 13q14 deletion (~50% of CLL cases) • Factors a/w worse prognosis include:
unfavorable cytogenetics (eg, 17p-/
TP
53 mutation)
unmutated (<2% c/w germline)
IgVH
gene (<8–10 y vs. >20–25 y if mutated)
high (>20–30%) Zap-70 expression (part of T cell receptor; correlated w/ unmutated
IgVH
)
CD38 >30% or CD49d <30% (correlated with unmutated
IgVH
)
higher β
2
-microglobulin levels (correlate with disease stage and tumor burden)
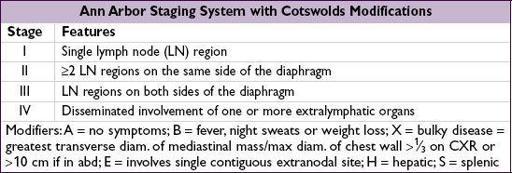
LYMPHOMA
Definition
• Malignant disorder of lymphoid cells that reside predominantly in lymphoid tissues •
Hodgkin lymphoma
(HL) is distinguished from
non-Hodgkin lymphoma
(NHL) by
the presence of
Reed-Sternberg
(RS)
cells
Clinical manifestations
• Lymphadenopathy (nontender)
HL
: superficial (usually
cervical
/
supraclavicular
) ± mediastinal lymphadenopathy;
nodal
disease with
orderly
,
anatomic spread
to adjacent nodes
NHL
: diffuse;
nodal and extranodal
disease with
noncontiguous spread
; symptoms reflect involved sites (abdominal fullness, bone pain)
• Constitutional (“B”) symptoms:
fever
(>38°), drenching
sweats
, ↓
weight
(>10% in 6 mo)
HL
: periodic, recurrent “Pel-Ebstein” fever; 10–15% have pruritus; ~35% “B” symptoms
NHL
: “B” symptoms vary between types, ~15–50%
Diagnostic and staging evaluation
• Physical exam: lymph nodes, liver/spleen size, Waldeyer’s ring, testes (~1% of NHL), skin • Pathology:
excisional lymph node bx
(not FNA b/c need surrounding architecture) with immunophenotyping and cytogenetics;
BM
bx (except in HL clinical stage IA/IIA with favorable features or CLL clone by flow); LP if CNS involvement clinically suspected • Lab tests: CBC, BUN/Cr, LFTs, ESR, LDH, UA, Ca, alb; ✓ HBV & HCV (and must ✓ HBsAg & anti-HBc if planning rituximab Rx as can lead to HBV reactivation); consider HIV, HTLV, & EBV serologies and connective tissue diseases autoAbs • Imaging:
chest/abd/pelvic CT
, but doesn’t reliably detect spleen/liver involvement
consider
PET-CT scans
(esp. in HL, DLBCL). PET response to Rx can be prognostic (
Blood
2006;107:52;
JCO
2007;25:3746); has role to assess PR/CR after treatment.
Head CT/MRI
only
if neurologic symptoms.
HODGKIN LYMPHOMA (HL) (
NEJM
2010;363:653)
Epidemiology and risk factors
• ~9,000 cases/y; bimodal distribution (15–35 & >50 y); ↑; role of EBV in subsets of HL, esp. immunocompromised patients
Pathology
• Affected nodes show RS cells (<1%) in background of non-neoplastic inflammatory cells • Classic RS cells: bilobed nucleus & prominent nucleoli with surrounding clear space (“owl’s eyes”). RS cells are
clonal B-cells
: CD15+, CD30+, CD20– (rarely +).
Other books
Omegasphere by Christopher John Chater
Ebony & Ivory Erotic Tales: Art Festival by Loveless, Mia
The Wedding Dress by Mary Burchell
LACKING VIRTUES by Thomas Kirkwood
La profecía by David Seltzer
From a Town on the Hudson by Yuko Koyano
The Music of Razors by Cameron Rogers
Philadelphia's Lost Waterfront by Harry Kyriakodis
Blood Games by Richard Laymon
Niagara Motel by Ashley Little