Breast Imaging: A Core Review (38 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine

B. A 2-mm cluster of pleomorphic microcalcifications in the central breast
C. Microcalcifications in the axillary tail region of the breast
D. A 3-cm segmental area of linear branching calcifications in the upper inner quadrant at a middle depth
36
A 31-year-old pregnant patient is discovered during her first trimester to have a breast cancer. The treatment for her breast malignancy is
A. None until after delivery
B. Immediate radiation therapy
C. Immediate chemotherapy
D. Immediate surgical resection
37
Which one of the following pathology results would most likely be considered discordant with the imaging findings of an irregular spiculated mass?
A. Postsurgical lumpectomy scar
B. Radial scar
C. Tubular carcinoma
D. Pseudoangiomatous stromal hyperplasia
ANSWERS AND EXPLANATIONS
1
Answer D.
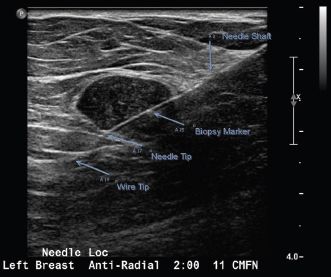
The needle used in this case was a 5-cm rigid needle and J wire. The hook wire needle system is more commonly used. Both needle systems would look similar during the localization process. The difference between the two systems is with the hook wire system the needle is removed, leaving only the wire in the patient for surgery. The advantage is the patient does not have a needle in her breast as she awaits surgery. With the rigid needle and J wire system, both the needle and the wire remain in the patient, the advantage being the wire and needle are less likely to be accidentally pulled out of position within the target or completely pulled out of the breast while the patient awaits surgery. In this case, A is the needle shaft, B is the biopsy clip marker, C is the needle tip, and D is the wire tip. The needle is advanced completely through the lesion, and the wire is then advanced through the needle to ensure that the surgeon completely excises the entire lesion.
Reference: Berg WA, Birdwell RL, eds.
Diagnostic Imaging: Breast
. Salt Lake City, UT: Amirsys; 2008;V:2-20–V:2-21.
2
Answer D.
Placing the patient’s arm and shoulder through the hole in the table exposes more of the deeper breast tissues.
Reference: Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:966.
3
Answer A.
Care must be taken when performing ultrasound-guided breast biopsies on patient’s with deep lesions, especially given their supine position, to avoid directing the needle into the mediastinum or lung. Rolling the patient and approaching at an angle as well as lifting the lesion off the chest wall reduce the risk. Aiming for the periphery does not ensure the needle would not hit the chest wall and may actually increase sampling error. It is not enough to obtain the patient’s informed consent for risk of pneumothorax; the approach must be adjusted to minimize risk of pneumothorax. If biopsy cannot be performed safely with ultrasound guidance, stereotactic maybe a viable option as the lesion can be held in place off the chest wall.
Reference: Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:942–944.
4
Answer C.
Multiple studies have shown that unless the fluid aspirated is maroon or dark brown suggesting old blood and therefore suspicious for an intracystic process such as a papilloma or carcinoma, sending the fluid for cytologic analysis is of no benefit.
Reference: Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:948–949.
5
Answer B.
Stereo images are obtained by angling the x-ray tube 15 degrees to one side perpendicular to the film plane and then 15 degrees to the other side resulting in a 30-degree difference between the two.
Reference: Kopans D.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:960.
6
Answer C.
The dead space of the biopsy needle can be up to 1 cm; therefore, at least 1.5 cm beyond the biopsy site should be anesthetized. During stereotactic biopsy, you can inject from the deepest part of the breast next to the Bucky out to the skin.
Reference: Flowers CI. Breast biopsy: Anesthesia, bleeding prevention, representative sampling, and rad/path concordance.
Appl Radiol
2012;41:9–13.
7
Answer A.
Several studies confirm that breast biopsies are safe in patients on antiplatelet or anticoagulation therapy but not in patients taking clopidogrel.
Reference: Flowers CI. Breast biopsy: Anesthesia, bleeding prevention, representative sampling, and rad/path concordance.
Appl Radiol
2012;41:9–13.
8
Answer D.
If the pathology report is negative, an x-ray in two planes—AP and lateral—of the specimen blocks can be performed. It is important to give the pathologist specific details about which block contains the calcifications and at what depth they are located. If calcium oxalate crystals are present, they are best seen under polarized light.
Reference: Flowers CI. Breast biopsy: Anesthesia, bleeding prevention, representative sampling, and rad/path concordance.
Appl Radiol
2012;41:9–13.
9
Answer B.
Topical lidocaine is available as viscous lidocaine or as a eutectic mixture of local anesthetics cream (EMLA) and can be applied 30 minutes prior to a subareolar mass procedure or for a ductogram.
Reference: Flowers CI. Breast biopsy: Anesthesia, bleeding prevention, representative sampling, and rad/path concordance.
Appl Radiol
2012;41:9–13.
10
Answer C.
The distance of shift allows for calculation of the lesion depth with respect to the center of rotation.
Reference: Carr JJ, Hemler PF, Halford PW. Stereotactic localization of breast lesions: How it works and methods to improve accuracy.
Radiographics
2001;21:463–473.
11
Answer E.
In most patients with history of breast cancer, imaging demonstrates thoracic changes resulting from treatment, complications of treatment, or tumor recurrence or metastasis. The postsurgical imaging appearance of the chest wall depends on the surgical method used (radical mastectomy, modified radical mastectomy, breast-conserving surgery, or breast reconstruction). The most common surgery-related complication is seroma. Radiation therapy frequently causes radiation pneumonitis, which occurs ~4 to 12 weeks after the completion of therapy, and is characteristically limited to the field of irradiation. Chemotherapy-related complications include cardiotoxicity, pneumonitis, and infection.
Reference: Jung JI, Kim HH, et al. Thoracic manifestations of breast cancer and its therapy.
Radiographics
2004;24(5):1269–1285.
12
Answer C.
Change the
x
and
y
coordinates after retargeting the lesion. By adjusting the
x
and
y
coordinates after retargeting a lesion that is too far away from the needle to be adequately sampled, a second skin opening or incision can be avoided. This adjustment can be performed by withdrawing the tip of the needle so that it remains through the skin.
Reference: Kopans DB.
Breast Imaging
. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:966.
13a
Answer D.
Although fine linear calcifications are considered suspicious, the next appropriate step is additional mammographic imaging with diagnostic workup.
Reference: Comstock CH, D’Orsi C, Bassett LW, et al.
Expert Panel on Women’s Imaging-Breast. ACR Appropriateness Criteria® Breast Microcalcifications—Initial Diagnostic Workup
. Reston, VA: American College of Radiology (ACR); 2009:12.
13b
Answer A.
Incomplete needs additional imaging. Further evaluation with diagnostic mammography should be performed prior to biopsy.
Reference: Comstock CH, D’Orsi C, Bassett LW, et al.
Expert Panel on Women’s Imaging-Breast. ACR Appropriateness Criteria® Breast Microcalcifications—Initial Diagnostic Workup
. Reston, VA: American College of Radiology (ACR); 2009:12.
13c
Answer D.
Tissue sampling of the most anterior and most posterior extent of the calcifications with stereotactic biopsy is the next appropriate step.
Reference: Comstock CH, D’Orsi C, Bassett LW, et al.
Expert Panel on Women’s Imaging-Breast. ACR Appropriateness Criteria® Breast Microcalcifications—Initial Diagnostic Workup
. Reston, VA: American College of Radiology (ACR); 2009:12.
14
Answer E.
After breast-conserving surgery, radiation therapy helps to control the microscopic disease, which has a comparable overall survival rate to mastectomy. Contraindications of whole breast irradiation include pregnancy, previous radiation, multicentric or diffuse disease, collagen vascular disease, and poor cosmetic outcome. Axillary lymphadenopathy is not a contraindication.
Reference: Ikeda D.
Breast Imaging: The Requisites
. 2nd ed. St. Louis, MO: Elsevier Mosby; 2011:233, box 8–3.
15
Answer D.
According to the published guidelines by the American College of Radiology and the American College of Surgeons, among others, the following are absolute contraindications to breast-conserving therapy: early pregnancy (first or second trimester) as radiation cannot be administered during pregnancy; women with two or more primary tumors in different quadrants; or women with diffuse malignant-appearing microcalcifications, prior irradiation to the same area of the affected breast, and persistent positive margins after reasonable surgical attempts. Relative contraindications include collagen vascular disease, large tumors in women with small breasts where good cosmesis could not be obtained with lumpectomy, and women with very large pendulous breasts for whom consistent, reproducible radiation fields would be hard to obtain. If breast cancer is diagnosed in the third trimester of pregnancy, breast-conserving therapy can be considered as radiation could commence after delivery.
Reference:
ACR-ACS-CAP-SSO Practice Guideline for Breast Conservation Therapy in the Management of Invasive Breast Carcinoma
; 2006.
http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/Invasive_Breast_Carcinoma
16
Answer B.
The most appropriate next step is recommendation for surgical biopsy. A critical part of image-guided breast biopsy is the follow-up of pathology results to determine whether pathology results are concordant with the imaging findings. The pathology results of “benign, fibrocystic changes with microcalcifications” are discordant with the imaging findings of this example. The morphology of these calcifications is linear and branching, which has a higher probability of malignancy, such as a BI-RADS 4B or 4C classification. Fine linear– or linear–branching calcifications are of higher suspicion for ductal carcinoma in situ (DCIS). The benign core biopsy result of fibrocystic change would be considered discordant with the imaging findings. Imaging–histologic discordance is an indication for surgical excision due to potential percutaneous undersampling. Therefore, the next most appropriate step would be referral to a surgeon for surgical biopsy of the calcifications. A more thorough sampling of the calcifications is in order to evaluate for malignancy. Answer choices A and C are incorrect. A 12- or 6-month follow-up mammogram is not appropriate for this case since the pathology results are discordant with imaging findings and the calcifications were likely inadequately sampled. Answer choices D and E are incorrect. A reattempt at stereotactic biopsy or breast MRI are not advised because they are not effective uses of time or resources. Definitive surgical biopsy is indicated.
Other books
A Sensitive Kind of Murder (A Kate Jasper Mystery) by Girdner, Jaqueline
TemptedByHisKiss by Tempted By His Kiss
Sleeping with the Dictionary by Mullen, Harryette
TMI by Patty Blount
LUST: A Bad Boy and Amish Girl Romance (The Brody Bunch Book 2) by Valentine, Sienna
The Boss's Pet: Sharing Among Friends by Kinzer, Tonya
Agentes del caos by Norman Spinrad
The Boy in the Suitcase by Lene Kaaberbol
The Longest Winter by Harrison Drake
Firefly Rain by Richard Dansky