i bc27f85be50b71b1 (248 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

APPENDIX III-A: MEDICAL -SURCICAL EQUIPMENT fN THE AClITE CARE SITTING
791
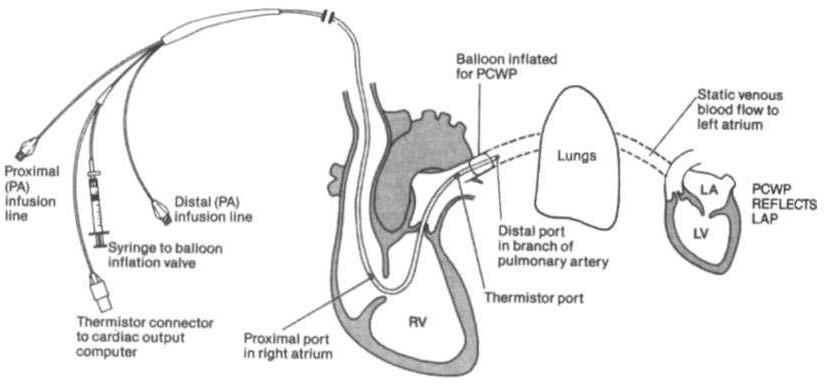
Figure IU-A.9. Pulmonary artery {PAl catheter (four lumen model) in a
branch of a PA with the bal/oon inflated; the pulmonary capillary wedge pres·
SlIre (peWP) ref/ects left atrial pressllre (LAP). (LA = left atrillm; LV = left
ventricle; RV= right vemricle.) (Reprinted with permission from LD Kersten
led/. Comprehensive Respiratory Nursing: A Decision·Making Approach.
Philadelphia: Sallllders, 1989;758.)
lotracranial Pressure Monitoring
Intracranial pressure (ICP) and cerebral perfusion pressure may be
measured in a variety of ways, depending on how urgently ICP values
are needed and the patient's neurologic or hemodynamic stability.
Refer to Intracranial and Cerebral Perfusion Pressure in Chapter 4 for
a description of these terms, Table 4-20 for a description of the early
and late signs of increased ICP, and Table 4-21 for a list of treatment
options to decrease ICP.
Table lll-A.S describes the different types of ICP monitors. For some
lCP monitors, such as the inrravenrricuJar catheter, the sensor and the
transducer must be level. Often, the zero point for the transducer is at the
traglls, or the top of the ear. A normal ICP waveform has a triphasic sinusoidal waveform and should correspond to heart rate.
General Physical Therapy Considerations with
Intracranial Pressure Monitoring
•
As with hemodynamic monitoring, be aware of the lCP value and
the corresponding waveform on the monitor. The waveform may
change shape (plateau wave) if cerebral hypoxia or ischemia occurs.1J

Table OJ-A.S. Intracranial Pressure (ICP) Monirors
.....
'"
N
Device
Description
Clinical Implications
Epidural sensor
Purpose: to monitor fCP.
§
•
The transducer does not need [Q be adjusted
Consists of: a fiberoptic sensor. It is placed
(releveled) with position changes.
()
>-
"
in the epidural space (i.e., superficial ro
•
Fair reliability.
'"
the dura) and connects to a transducer
J:
>and monitor.
Z
o
Subarachnoidl
Purpose: ro directly monitor ICP and provide
•
The physician will determine the level to which the
g
subdural bol,
access for CSF sampling.
transducer should be positioned. This is documented
"
Consists of: a bolt or screw placed in the
in the chart and posted at me bedside.
"
"
subarachnoid or subdural space through a
•
The transducer must be repositioned to the
�
J:
burr hole.
appropriate level with position changes.
-<
�
•
Poor reliability.
�
Intraventricular
Purpose: to directly monitor ICi> and provide
r
•
The nondominant hemisphere is the preferable
catheter
access for the sampling and drainage of
insertion site.
J!
'"
"
(ventriculosromy)
CSF. Occasionally used to administer
•
There are twO different types of drainage
>
medications.
systems: intermittent and continuous.
�
Consists of: a small catheter that is placed in
•
The intermittent system allows the nurse to drain
the anterior horn of the lateral ventricle
CSF for 30-120 secs by momentarily opening a
through a burr hole. The catheter connects
stopcock when the lCP exceeds the parameters set
to a transducer and to a drainage bag,
by 'he physician.
where CSF collects.
•
A continuous system allows the drainage of CSF to
occur against a pressure gradient when the
collection bag is positioned (leveled) above [he
foramen of Monro. This is usually 15 cm above the
external auditory meatus.


,.
• The transducer must be repositioned to the
�
appropriate level with position changes.
'Z
'"
• Very reliable.
x
Fiberoptic transducer
Purpose: co monicor fCP. Can also monitor
• The transducer does not need to be adjusted
tipped catheter
incraparenchymal pressure (if the catheter
(releveled) with position changes.
;:
is placed in the parenchyma).
•
Very reliable.
b
Consists of: a fiberoptic transducer-tipped
9
catheter. It is placed in the venrricle, within
r
J,
the parenchyma, or in the subarachnoid or
C
"
subdural space.
Cl
l'
>
CSF
r
= cerebrospmal fluid.
Sources: Data from A£ Davis, TL Briones. Intf3cranial Disorders. In MR Kinney, S8 Dunbar, JM Virello-Cicciu) et al. (cds), AACN's Clinical E
c
Reference Manual for Critical Care Nursing (4th cd), St. Louis: Mosby, 1998; and LA Thelan, KM Stacy, LD Urden, ME Lough (cds). Neuro
;;
l::
logic Therapeutic Management, Critical Care Nursing: Diagnosis and Managemem (3rd ed). St. Louis: Mosby, 1 998.
�
z
J!
"'
>
n
!OJ
"'
n
,.
'"
"'
�
"
'"
'"
7 94 ACtJrE CARE HANDBOOK FOR PHYSICAL THERAPISTS
•
Momentary elevations in ICP will normally occur. It is a sustained elevation in ICP that is of concern and should be reported to the nurse.
•
Patients with elevated ICP are often positioned with the head
of the bed at 30 degrees, which maximizes venous blood flow
from the brain to help decrease ICP.'4 Therefore, be aware that
lowering the head of the bed may increase ICP. Other positions
that increase ICP are the Trendelenburg position, lateral neck
flexion, and extreme hip flexion.
•
Additional conditions that increase ICP are the Valsalva maneuver, noxious stimuli, pain, and coughing.
Medical-Surgical Management Devices
Different lines, tubes, catheters, and access devices comprise the wide
variety of medical-surgical equipment used in the acute care setting.
In general, these devices may be peripheral or central, for shorr- or
long-term use, and inserted or applied at the bedside in a special procedure (e.g., under fluoroscopic guidance) or in the operating room.
Table LII-A.6 describes the medical-surgical management devices most
commonly encountered in the acute care setting.
General Physical Therapy Considerations with
Medical-Surgical Management Devices
The following clinical tips apply to medical-surgical equipment, as
well as to the 02 therapy and noninvasive, invasive, and ICP moniroring equipment previously discussed.
Clinical Tip
•
Before entering a patient's room, review the medical
record, particularly new orders, recent progress notes, and
test results. Review graphic sheets for vital signs, noting
trends or variations from the norms.
•
Note whether any particular precautions protecting the
patient or the caregiver from specific pathogens are in