In the Midst of Life (51 page)
Read In the Midst of Life Online
Authors: Jennifer Worth

‘I want to take her home to die,’ I stuttered.
‘It’s not an option now,’ replied the doctor. ‘I cannot discharge her like this, so close to death.’
It was a truly desperate feeling watching my mother dying,
aching to swing into action and ‘do my paramedic stuff,’ when, deep inside, I knew there was absolutely nothing I could do to prevent the inevitable slide into death. Mum’s was as dignified as it could be in the little side room. Both Matthew and I held her hands and watched as her breathing slowly began to fail – when we were finally able to rid her of the oxygen mask – and saw the peaceful look come over her face when her exhausted heart eventually stopped beating.
It gave us both a whole new perspective on death and how it affects those it leaves behind.
We both returned to work, vowing to look into the end-of-life care policies our respective ambulance trusts had in place.
As a coincidence, in June 2008, the Darzi Report was issued by the Department of Health, with the title
High Quality Care for All.
Some of the concerns raised by Lord Darzi included those surrounding end-of-life care. I happened to glimpse some information on this review and begged my Chief Executive Paul Sutton to consider the possibility of championing end-of-life care for SECAMB NHS Trust. He was enthusiastic about my interest, and, with his encouragement, I attended a conference on the subject in November, and found it extremely engaging.
On the back of that conference – and by talking and writing to some of the speakers and delegates – I was invited to speak at the National Council for Palliative Care conference at Guy’s Hospital in March 2009 on the subject of ‘Dying Differently’. My intention was to speak to the delegates and impress on them the fact that ambulance crews are not just there to perform CPR and dash the patient to hospital, but we can also have a place with palliative care patients, even if it is just to administer pain relief or oxygen.
In the past year our Trust has implemented a general policy surrounding Do Not Attempt Resuscitation and Advance Directive to Refuse Treatment. Any palliative care team can email our Trust with a copy of these orders, and we have the facility to add a history marker linked to an address where a palliative care patient lives, so if an emergency call is generated for that person, the
information is passed to the crew that the patient is not to be resuscitated.
Indeed, this facility also extends to GPs and hospital consultants who have patients who have requested DNAR for a variety of conditions – COPD (like my mother), advanced Alzheimer’s, Parkinson’s, or any other illness or condition where CPR is deemed inappropriate. The only thing we require to enable us to safeguard ourselves is the sight of the original unaltered document that is signed by the doctor on arrival at the call.
These DNAR documents have no expiry date and, once signed, are valid until the patient dies or the order is changed for whatever reason.
DNAR in most cases would refer to CPR only, but also has the flexibility to allow withholding other treatment such as artificial nutrition and hydration – although these treatments tend to apply to patients already in hospital. Other ambulance services are working around the Allow a Natural Death (AND) procedure.
What is encouraging, of course, is that the ambulance service is now very much part of the integrated multi-disciplined team, and is consulted by the various primary care trusts in end-of-life care issues; and our concerns and wishes are being registered and used, helping us all with the treatment and services we can offer to patients as they reach the end of their natural lives.
What the future holds
Advancement in training, education, and the ever-increasing policies and protocols we follow now, will no doubt lead to an older, and healthier, nation. It is an amazing fact that treatments that we currently use already lead to heart attack and stroke patients recovering fully and going back to ‘tax paying’ status in a few short weeks. Twenty years ago, these patients would have died, or become paralysed for the rest of their lives.
I often chat with my work colleagues and ask them the searching question, ‘Have you thought about how and where you would prefer to die?’
I am surprised that most of them haven’t even thought about
their own death, or what their personal preference is. This alarms me, considering the amount of death we actually deal with in our line of work!
For my own part, should I be suffering from an incurable illness, I will be instructing my GP and get my own DNAR written out, and I will leave it in a big white envelope just by the front door - in the hope that the young, keen ambulance crew who come rushing in will take note, and leave me to die in the peace I hopefully have earned!
Should
patients at the end of life be given the option of receiving CPR?
by Madeline Bass, BSc, RGN, Head of Education, St Nicholas Hospice, Bury St Edmunds, Suffolk
First published in
Nursing Times;
105 4, 26-02-2009.
Cardio-pulmonary resuscitation (CPR) is often unsuccessful and may not always be appropriate at the end of life. This article debates whether the use of cardio-pulmonary resuscitation by healthcare professionals in situations when it is unlikely to be successful feeds an unhealthy appetite to intervene just because it is possible. It explores the problem of offering patients and relatives the choice about CPR at the end of life when it is likely to be unsuccessful.
End-of-life and palliative care has become an increasingly important area of healthcare professionals’ work following publication of the End of Life Care Strategy (Department of Health, 2008).
Good communication between patients and staff is essential for those who are making choices and decisions about care at the end of life. This may include discussions about cardio-pulmonary resuscitation.
We can now treat disease and disability in ways that would not have been thought possible sixty years ago. These achievements have also created bioethical dilemmas. The advent of new treatment interventions has brought its own unhealthy appetite - the more treatments healthcare workers have to offer, the more they intervene. To them, this equates with doing the best for patients and knowing that everything has been tried.
However, in some cases, interventions can mean poor outcomes
for the patient and result in low staff morale. One area of particular concern is the decision about when it is appropriate to perform CPR.
Misconceptions about CPR
The media’s interpretation of CPR, primarily through TV drama, has led to a misunderstanding that it is a quick intervention that guarantees success without any side-effects (Bass, 2003; Diem
et al,
1996).
CPR was first used in its present advanced life-support format of chest compressions, ventilation and defibrillation in i960 (Kouwenhoven
et al,
1960). The main problem associated with CPR is identifying when it is appropriate to instigate it as a life-saving measure. The concern is that the decision to proceed is often viewed as the default if a decision about resuscitation has not been made.
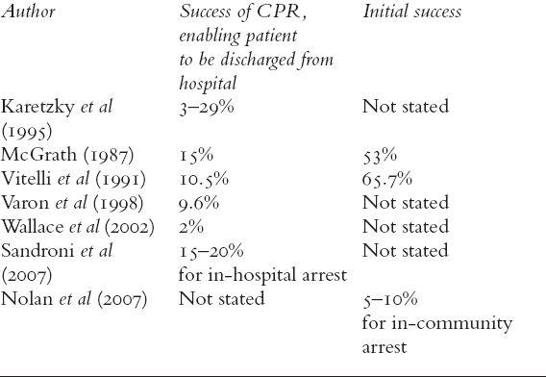
CPR was devised as an emergency intervention for unexpected cardiac or respiratory arrest (Kouwenhoven
et al,
i960) and the majority of healthcare professionals are not aware that the success rates for CPR are very low (Wagg
et al,
1995; Miller
et al,
1993) (see Table 1). Only a small percentage of people will survive to leave hospital following a cardiac or respiratory arrest.
Ewer
et al
(2001) looked at the success rates of CPR undertaken on patients with cancer. They asked whether patients were expected to have an irreversible cardiac or respiratory arrest. The results showed that, of patients having an unexpected, reversible arrest, there was a 22.2% success rate. However, for those who were expected to have an irreversible arrest and were at the end of life, there was 0% success.
The effects of inappropriate CPR are often not considered. These include post-resuscitation disease (complications caused by resuscitation itself) (Negovsky and Gurvitch, 1995), an undignified death for the patient, and distress to relatives. Paramedics and resuscitation teams may also become demoralised by repeated failures (Jevon, 1999).
Table
1
. Success rates for CPR
Factors influencing success of CPR
The success of CPR is often measured in terms of initial success - the return of heartbeat and breathing, controlled independently by the patient. It is also measured in terms of survival to discharge (see Table 1). The chances of successful CPR are improved if
- There is early access to a cardiac arrest team
- Basic life support is commenced immediately
- Defibrillation is carried out as quickly as possible in cases of ventricular tachycardia or pulseless ventricular fibrillation (Jevon, 2002).
Other positive factors associated with a successful CPR attempt include:
- A non-cancer diagnosis
- Cancer without metastases
- The patient is not housebound
- Good renal function
- No known infection
- Blood
pressure within normal range - The patient has robust health (Newman, 2002).
The Gold Standard Framework (GSF) suggests that cancer, organ failure, general frailty and dementia are not associated with success (NHS End of Life Programme, 2007).
The BMA
et al
(2007) recommended that CPR should not be attempted when patients have indicated before the cardiac arrest that they would refuse it or if the attempt is likely to be futile because of their medical condition.
Resuscitation decisions
Discussions about resuscitation at the end of life raise a number of questions.
- Are public expectations of healthcare and technology unrealistic?
- Do healthcare professionals pursue the possibility of an immediate positive outcome from CPR without considering the long-term consequences of the intervention?
- Does inappropriate CPR raise false hope in patients, relatives and staff? (Jevon, 1999)
Awareness and knowledge of CPR guidance among healthcare professionals is poor (Bass, 2003), with knowledge focusing on local policy rather than research evidence and national guidance.
In addition, healthcare professionals often fail to recognise when a patient is dying, which can result in difficulty making an appropriate decision about whether to resuscitate in the event of a cardiac or respiratory arrest. The Liverpool Care Pathway (LCP) is a recommended national tool that can assist professionals to make an accurate diagnosis of dying (Ellershaw and Ward, 2003). This diagnosis can help to inform discussion about when to initiate CPR.
Reducing the inappropriate use of CPR
The inappropriate use of CPR can be reduced by improving
communication between all members of the multidisciplinary team. The End of Life Care Strategy (DH, 2008) gives guidance and outcomes for care at the end of life, including dignity, appropriate care and comfort – appropriate care should include refraining from undertaking inappropriate CPR.
The Mental Capacity Act 2005 allows patients to make advance care plans and allows them to have choices at the end of life. If they are to support patients in making such plans, healthcare professionals need to discuss appropriate choices with them.
It is good practice to have a local Do Not Attempt Resuscitation (DNAR) policy, and use the documentation from the GSF for patients in their own home. The framework prompts healthcare professionals to initiate discussions around advance care planning, such as about what patients want at the end of their life and whether they have choices.
The GSF also encourages healthcare professionals to ask the question: ‘Would I be surprised if this person died in one year/one month/one week/one day?’ The patient is coded and specific guidance for this coding is given. The coding is:
A: prognosis of years
B: prognosis of months
C: prognosis of weeks
D: prognosis of days.
Guidance relating to the coding provides information about what professionals should discuss with patients and care that should be planned and provided.