The End of Diabetes (4 page)
Read The End of Diabetes Online
Authors: Joel Fuhrman

In contrast, type 2 diabetics can become nondiabetic, achieving complete wellness and even excellent health. They can be diabetes-free for life. In my twenty years of clinical experience with this program, I have experienced that more than 90 percent of type 2 diabetics who follow this diet and exercise lifestyle are able to discontinue insulin within the first month.
Jim Kenney, a fifty-eight-year-old male, was referred to my office from his nephrologist (kidney specialist) at St. Barnabas Hospital in Livingston, New Jersey. He was originally referred to the nephrologist by his endocrinologist (diabetic specialist) at the Joslin Diabetes Center in Boston because of kidney damage that resulted from very high glucose readings in spite of maximum medical management. At this first visit, Jim weighed 268 pounds and was on 175 units of insulin per day (a very high dosage). He had already suffered from severe complications of type 2 diabetes, including two heart attacks and Charcot (destructive inflammation) joint damage in his right ankle. In spite of this huge dose of insulin and six other medications, Jim's glucose readings averaged between 350 and 400. Jim said this was the case no matter what he ate, adding that he was already on a diabetes diet and was already following the precise diabetes nutrition and dietary recommendations of the dietician at the Joslin clinic.
During his first visit with me, after we discussed his new diet program, I reduced his insulin dose to 130 units per day. The following few days, Jim and I spoke over the phone, and I continued to decrease his insulin gradually. Within five days, Jim's glucose was running between 80 and 120 and he lost ten pounds. At this juncture I reduced his Lantus long-acting insulin dose to 45 units at bedtime and his Humalog regular pre-meal insulin to 6 units per meal, for a total of 63 units per day.
At his two-week visit, Jim had lost sixteen pounds. I was already stopping some of his blood pressure medications and he was down to a total of 58 units of insulin per day. After the first month, I was able to stop all of Jim's insulin and start him on Glucophage (metformin). He lost twenty-five pounds in the first five weeks, and his blood glucose readings were well controlled without insulin. In addition, his blood pressure came down to normal, he no longer required any blood pressure medications, and his abnormal kidney function was improving. Five months later, Jim had lost sixty pounds and was off all medications for diabetes. He no longer had high cholesterol or high blood pressure. His kidney insufficiency had completely normalized as well.
Jim's story illustrates not merely how powerful this dietary protocol is but also how the standard nutritional advice given to diabetics from conventional physicians and dieticians can be disease promoting. The standard nutritional advice given to diabetics is not only insufficientâit is dangerous. Jim Kenney would likely be dead by now had his nephrologist not referred him to my office.
T
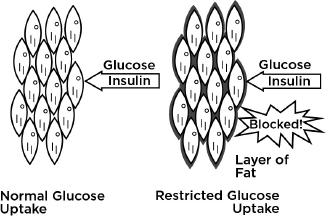
o begin examining how type 2 diabetes can be healed, we need to look at how it developed in the first place. As mentioned, the heavier you are, the greater your risk of developing type 2 diabetes. For some people even a small amount of excess fat on the body can trigger diabetes. Your body's cells are fueled primarily by glucose. Insulin is the hormonal messenger produced by the beta cells in the pancreas, which induces glucose uptake into the body's cells. Glucose cannot pass into the cells unless insulin opens the gate. However, as little as five pounds of excess fat on your frame can interfere with insulin's ability to carry glucose into your cells. When you have excess fat on your body, insulin does not work as well, and then the glucose has difficulty entering the cells. Fat on the body interferes with the action of insulin through multiple mechanisms.
Free fatty acids released from the fat cells is one of the mechanisms promoting insulin resistance in liver and muscle in a phenomenon known as lipotoxicity. The excess of circulating fats in the bloodstream also blocks insulin binding on the outer membrane of cells and interferes with normal muscle cell function and energy production. When cellular energy production is slowed, more insulin is required. This lipotoxicity can affect the heart as well, promoting an irregular heart beat and increasing susceptibility to heart failure.
Fat cells also produce binding proteins that attach to the insulin hormone blocking its activity. Some of these fat cellâproduced molecules also cause muscle cells to be desensitized to insulin. If that is not bad enough, when our cell membranes are impregnated with dietary trans fats and saturated fats, the insulin-binding sites are distorted, impairing insulin from binding to the docking station on the cell membranes, making insulin less effective at enabling glucose uptake. To overcome all these issues, your pancreas must produce additional insulin. With significant weight gain, the insulin-producing beta cells in the pancreas become dramatically overworked. In short, type 2 diabetes is a disease of heightened insulin
resistance,
not one of absolute insulin
deficiency.
Insulin works less effectively when people eat fatty foods, overeat, eat low-nutrient foods, or gain weight. So when people are overweight, they require more insulin, whether they're diabetic or not. But giving overweight diabetic people even more insulin makes them sicker by promoting further weight gain, causing them to become even more diabetic. How does this process work? Our pancreas secretes the amount of insulin demanded by the body. People of normal weight with about one-third of an inch of periumbilical fat will secrete a certain amount of insulin. But what happens when they gain twenty pounds of fat? Their bodies will now require more insulin, almost twice as much, because the fat on their bodies interferes with the uptake of insulin into the cells by the various mechanisms mentioned.
Â
Body Fat Deactivates Insulin and Raises Blood Glucose
â¢Â Free fatty acids circulating in the blood have a toxic effect, inhibiting energy production from muscle tissues, which then demand more insulin.
â¢Â Fat cells produce pigment epithelium-derived factor, causing cells to be desensitized to insulin.
1
â¢Â Fat cells produce retinol-binding protein, which prevents insulin from activating glucose-carrying proteins.
2
â¢Â Trans fats and saturated fats can stiffen and distort membrane-located insulin receptors, interfering with efficient binding.
3
Â
When people are significantly overweight or obese, with more than fifty pounds of excess fat weight, their bodies demand huge loads of insulin from the pancreas, even as much as ten times more than people of normal weight require. What do you think occurs after ten or more years of overworking the pancreas so hard? Of course, it becomes exhausted and loses the ability to keep up with the huge insulin demands, and less insulin is produced. Eventually, with less insulin available to move glucose from the bloodstream into the cells, the glucose level in the blood starts to rise, and those people are diagnosed with diabetes. In most cases, these people are still secreting an excessive amount of insulin, compared to a normal-weight people, but just not enough for them. As time goes on, even though the overworked pancreas may still pump out much more insulin than a thinner person might need, it won't be enough to overcome the effects of the disease-causing body fat. I call it pancreatic poop out.
Some severely overweight individuals have a large pancreas beta cell capacity, so they can produce high levels of insulin without becoming diabetic. These high insulin levels in the blood are a strong predictor of heart attack risk and life span. So whether these people are diabetic or not, their high insulin levels are still dangerous. In fact, insulin level is a better indicator of a future heart attack than cholesterol level. Often people will be in an emergency room with their first heart attack and be told for the first time that their sugar is elevated. These heart attack victims never knew they had diabetes. The first sign of it was the heart attack from years of having a heightened insulin level. Damage was building up before the elevated glucose became apparent.
In most cases, the pancreas's ability to produce insulin continues to lessen as the diabetes and the overweight condition continue year after year. Unlike type 1 diabetes, total destruction of insulin-secreting ability almost never occurs in type 2 diabetes. But the sooner type 2 diabetics lose the extra weight that is causing the diabetes, the greater the likelihood they will be able to maintain a functional reserve of insulin-secreting cells in their pancreas.
What this means is that typical type 2 diabetes is caused by excess weight in individuals who have a smaller reserve of insulin-secreting cells in the pancreas
.
As the statistics are showing, type 2 diabetes is a growing epidemic. But what is surprising is that people suffering can range anywhere from ten pounds overweight to significantly obese. It is important to say here that in individuals who are susceptible, ten to twenty extra pounds can lead to diabetic symptoms
.
No matter what the number is, losing the excess weight enables these individuals to live within the capabilities of their body. Most type 2 diabetics still produce enough insulin to maintain normalcy as long as they maintain a favorable body-fat percentage.
Simply put, since the level of insulin in your blood is a good indicator of your risk for heart attack, and since a tape measure around your waist is nearly as good an indicator of insulin levels as a blood test, it makes sense to remember the ancient saying, “The longer your waistline, the shorter your lifeline.”
Following a nutrient-rich, lower-calorie dietâa nutritarian dietâcoupled with a good exercise program is the most important change you can adopt to extend your life span. It has been known for years that intentional weight loss improves blood sugar, lipids, and blood pressure in diabetics. Gastric bypass surgery and lapband procedures are risky, lead to malnutrition, and most often produce only temporary results. Nevertheless, overweight individuals who go through gastric bypass surgery and become too uncomfortable to eat much often also resolve their diabetes. Over the years, as the stomach stretches and the weight returns, these individuals can become diabetic again. Unfortunately, they did not learn enough about nutritional excellence. A recent study documented a significant increase in life span, with an average of 25 percent reduced mortality, when diabetic individuals dropped their body weight by just twenty to twenty-five pounds.
4
Imagine the results when a program of nutritional excellence achieves the weight loss and the body's cells are flooded with micronutrients that fuel cellular repair. Scientific literature shows it is not just the weight reduction that enables diabetic reversal and recovery but also the high level of plant-derived micronutrients and phytochemicals that can fuel the body's own remarkable self-healing properties.
5
The results you can achieve with a nutritarian diet are predictable and remarkable, but it takes some effort and time. There are lots of diet books and exercise plans written for diabetics, but this nutritarian diet is designed and proven in clinical practice to be the most effective for losing weight, lowering cholesterol, and reversing diabetes. It is the gold standard, written specifically for people who want to do what is very best for their health and give it their all to become nondiabetic.
A nutritarian approach is all about superior nutrition, not just moderate improvement in diet. Moderation doesn't work. But not to worryâas already mentioned, nutritional excellence will make your taste buds happy and you will be more than satisfied with the amount of food you can eat. But we will get into that later in the book.
Â
Decreasing Insulin and Other Medications
Type 2 diabetics are overweight to begin with and, as you have learned, being overweight is the significant causative factor in diabetes. Because insulin therapy results in further weight gain, how could giving more insulin or oral medication to force the already overworked pancreas to produce more insulin be a good thing? A vicious cycle begins that usually causes diabetics to require more and more insulin or other medications as they put on the pounds. On their initial visit to me, patients often report their sugars are impossible to control in spite of massive doses of insulin, which are typically combined with oral medication. These patients are significantly overmedicated but are still overweight and eating unhealthfully. It is like they are walking around with a live hand grenade, ready to explode at any minute.
Excess insulin in the same environment as excess weight, high cholesterol, hypertension, and inflammation from inferior micronutrient exposure promotes hardening of the arteries, which will eventually lead to heart attacks and strokes. Studies have shown that high levels of insulin in the blood promote hardening of the arteries even in nondiabetics. In diabetics, the effects of excess insulin are even worse. In a study of 154 treated diabetics, blood vessel disease was greatest in those with the highest levels of insulin.
6
It made no difference whether the insulin was self-produced in the body or taken by injection. Quite a few studies illustrate the dangers of giving insulin to type 2 diabetics. When these patients are given insulinâcompared with those given an oral antidiabetes medication, the risk of death from heart attacks tripled.
7