Thyroid for Dummies (12 page)
Read Thyroid for Dummies Online
Authors: Alan L. Rubin

08_031727 ch04.qxp 9/6/06 10:47 PM Page 49
Chapter 4: Testing Your Thyroid
49
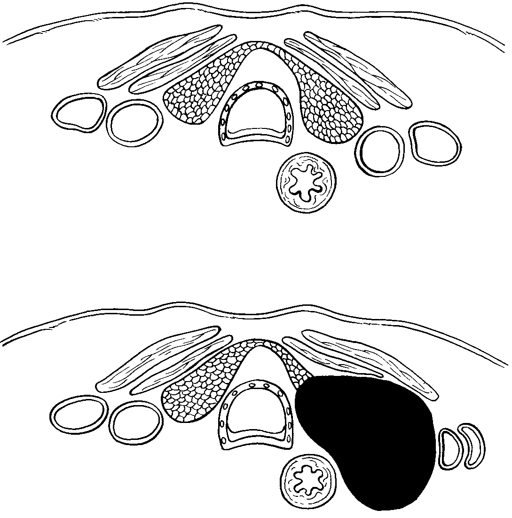
Normal ultrasound
Skin
Sternohyoid muscle
Sternothryoid muscle
Sternohyoid muscle
Trachea
Left jugular
Lobes of thyroid
Right jugular
vein
gland
vein
Left common
Oesophagus
carotid artery
Right common
carotid artery
Nodule shown on ultrasound
Figure 4-2:
A normal
ultrasound
study (top)
and an
ultrasound
that shows
a solid
nodule
(bottom).
Nodule on right thyroid lobe
Fine needle aspiration biopsy (FNAB)
When a doctor wants to know the type of tissue making up a growth on the thyroid, the
fine needle aspiration biopsy (FNAB)
is the definitive test. This test is virtually painless and is free of complications. A small needle is introduced into the growth, and tiny bits of tissue are sucked up (aspirated) by pulling back on the plunger to create a vacuum. The needle is moved to a few different places on the growth.
The aspirated tissue is sprayed on a fixative, stained, and examined for signs of cancer. This test is a fairly reliable method to establish whether the growth is cancerous or not. Occasionally, the tissue won’t provide a clear diagnosis, and the lobe (side) of the thyroid (refer to Chapter 3) that contains the lump is removed in an operation called, simply, a
lumpectomy
.
08_031727 ch04.qxp 9/6/06 10:47 PM Page 50
50
Part I: Understanding the Thyroid
FNAB has saved thousands of patients from surgery and is often the first test performed to check for cancer, skipping the thyroid scan and the ultrasound.
This approach is based on the Willie Sutton theory. Willie was a bank robber and was once asked why he robbed banks. His answer was ‘You go where the money is.’
Deciphering ultrasound
A beam of sound from an ultrasound device
sound back. Different tissues absorb the sound
consists of high frequency sound waves. The
differently; therefore, reflecting the sound to a
frequency is far higher than anything the human
different extent. A cancer appears differently on
ear can hear. When focused and directed, just
an ultrasound to a normal thyroid tissue or
like a beam of light, to strike tissue, the tissue
a cyst filled with fluid. When the reflection
reflects a certain amount of the sound beam
returns, the sound energy is converted to light
back – the amount depends upon the density of
energy and electrical energy. These signals are
the tissue. Air hardly reflects back any of the
then displayed on a cathode ray tube or, if a film
beam, while tissue, which is made up of many
is exposed to the light energy, made into a per-
layers and contains water, sends plenty of
manent record.

09_031727 pt02.qxp 9/6/06 10:45 PM Page 51
Part II
Treating Thyroid
Problems
"Now I'm getting better, they're taking
me off the radioactive iodine treatment."
09_031727 pt02.qxp 9/6/06 10:45 PM Page 52
In this part . . .
The thyroid can be overactive or underactive. It can be too large or too small. It can be bumpy or smooth. The chapters in this part introduce you to all kinds of thyroid abnormalities. You discover how to recognize them and how to differentiate one from another. For those of you with thyroid disorders, we explain how they occur, which of the common signs and symptoms you have, how a particular disorder damages your body, and what you can do to cure it so no damage occurs.
10_031727 ch05.qxp 9/6/06 10:46 PM Page 53
Chapter 5
Dealing with an
Underactive Thyroid
In This Chapter
ᮣ Understanding thyroiditis and hypothyroidism
ᮣ Determining the cause of low thyroid function
ᮣ Checking for other autoimmune conditions
ᮣ Treating hypothyroidism
Low thyroid function (also known as hypothyroidism or myxoedema) is the most common form of thyroid disease throughout the world.
Although the condition has numerous causes, iodine deficiency leads the list worldwide (see Chapter 12). In the United Kingdom and other parts of Europe, however, iodine deficiency is rare. The leading cause of hypothyroidism is the presence of an autoimmune thyroid disease. An autoimmune condition is one in which your own immune system attacks a part of the body, usually by producing antibodies that recognise and attack a body component such as the thyroid. Autoimmune thyroid conditions include
chronic
thyroiditis,
known also as
Hashimoto’s thyroiditis
or
autoimmune thyroiditis
, which is discussed in this chapter, and Graves’ disease (see Chapter 6).
(Check out Chapter 4 for a description of thyroid autoantibodies.) This chapter introduces you to the immensity of this problem, shows you how hypothyroidism affects the body, and explains the proper treatment for the various forms of hypothyroidism. In the last few years, key changes in our understanding of hypothyroidism have occurred, and that new information is included here, too, so you are up-to-date when you talk with your doctor about symptoms and treatment.
10_031727 ch05.qxp 9/6/06 10:46 PM Page 54
54
Part II: Treating Thyroid Problems
Living with Autoimmune Thyroiditis
Stacy, a 46-year-old woman, is the cousin of Sarah and Margaret, who are introduced in Chapter 2. Stacy is generally healthy but recently noticed some swelling in the lower part of her neck. The swelling seemed to develop very slowly, and she didn’t notice it until she tried to button a collar over her neck. Other than the swelling, she has really not had any physical problems.
Stacy isn’t gaining weight. She sleeps well at night and isn’t overly tired. She doesn’t feel unusually hot or cold. Her appetite is normal, as are her bowel movements. She has no discomfort associated with the growth in her neck.
Stacy’s cousin, Sarah, who was recently diagnosed with hypothyroidism, tells Stacy that, according to her thyroid specialist, other members of her family may develop thyroid disease, too. Stacy goes to see her GP, who examines her and finds that her thyroid gland is twice as large as normal. She finds no other significant abnormalities. She sends Stacy to the nurse for two blood tests – a thyroid-stimulating hormone (TSH) test and a free thyroxine (FT4) test – both of which return within the normal range (refer to Chapter 4).
Because of her clinical suspicion, Stacy’s GP also obtains thyroid autoantibody studies. These results are very elevated, particularly the thyroid peroxidase autoantibodies, but also the antithyroglobulin autoantibodies (discussed in Chapter 4).
Stacy’s doctor tells her that she has a condition called
chronic thyroiditis
. He tells Stacy that treatment at this time is optional. If she is unhappy with the swelling sticking out on her neck, she can take thyroid hormone and it will shrink. If not, she need only return in six months or a year to check whether the disease has progressed to hypothyroidism.
Stacy’s condition is a typical illustration of chronic thyroiditis. She is free of symptoms at this stage, and the only abnormality is her goitre, an enlargement of the thyroid gland. The blood tests that reflect thyroid function are normal. The high levels of thyroid autoantibodies in her system determine the diagnosis.
The extent of the problem
Most studies indicate that 10 per cent of the world’s population tests positive for thyroid autoantibodies (refer to Chapter 4). If the United Kingdom has a population of approximately 60 million people, around 6 million of them will test positive. Many experts believe that all these people have chronic thyroiditis, but the vast majority will never develop symptoms and the condition won’t bother them in any way.
10_031727 ch05.qxp 9/6/06 10:46 PM Page 55
Chapter 5: Dealing with an Underactive Thyroid
55
Only about 1 in 1,000 of people who test positive for thyroid autoantibodies develop symptomatic chronic thyroiditis, which means that about 6,000 new cases occur in the United Kingdom each year. A woman is 20 times more liable to develop
symptomatic
chronic thyroiditis – chronic thyroiditis where the symptoms actually show – than a man. The typical patient is 30 to 50
years old, but chronic thyroiditis is also found in children.
Chronic thyroiditis is a familial disease that is usually transmitted from mother to daughter. Even members of the family who show no symptoms often have thyroid autoantibodies in their blood (especially the females).
They may develop hypothyroidism later on.
Symptoms of chronic thyroiditis
Some people with chronic thyroiditis do have symptoms, even when their thyroid function tests are normal. In addition to neck swelling, symptoms include:
ߜ Pain in the neck (which is unusual)
ߜ Chest pain (which occurs in about 25 per cent of patients) ߜ Sensation of fullness in the neck and sometimes, trouble swallowing ߜ Transient symptoms of hyperthyroidism (see Chapter 6) – but blood tests are not normal when these short-term symptoms occur Approach to treatment
As the condition is so benign, chronic thyroiditis that has not progressed to hypothyroidism is usually not treated. If you have neck pain because of chronic thyroiditis, it’s generally controlled with aspirin or paracetamol. If the swelling in your neck is unsightly, or you have difficulty swallowing, your doctor can prescribe thyroid hormone to block the production of thyroid-stimulating hormone (TSH). Your thyroid gland then shrinks. Your doctor may suggest stopping hormone treatment at some later date, and review you regularly, as one-quarter of patients with this condition have a remission and no longer need thyroid treatment.
If you experience transient symptoms of hyperthyroidism as a result of chronic thyroiditis, these symptoms usually require no treatment either. The symptoms usually last a few weeks, and then you return to normal. In especially severe cases, drugs that block the action of thyroid hormones (see Chapter 6) are used.
10_031727 ch05.qxp 9/6/06 10:46 PM Page 56
56
Part II: Treating Thyroid Problems
Identifying Hypothyroidism
Karen is Stacy’s younger sister. Over the last few years, she has noticed a gradual enlargement of her neck – a symptom similar to the one that Stacy experienced. But Karen has had a number of other problems as well. She has gained a few pounds, and her legs appear swollen but do not retain an indentation when she presses on them. She feels cold when her husband feels comfortable and is constantly asking for more heat. Her skin is dry and her nails are brittle. She has dry hair and notices that she is losing more hair than before. The outer third of her eyebrows seems to have disappeared, along with some of her eyelashes. She used to love to sing in the church choir, but her voice is now too husky. She has trouble seeing to drive at night and notices trouble hearing as well.
Her GP, who is familiar with the family’s thyroid problems, examines her in her surgery. She finds that, in addition to all the symptoms Karen explains to him, she also has a slow pulse and an enlarged thyroid gland. She sends her for thyroid function tests (TSH and FT4) as well as thyroid autoantibody tests.
Karen’s tests show that she has a low FT4, a high TSH and her autoantibody levels are elevated. The doctor makes a diagnosis of hypothyroidism due to chronic thyroiditis and starts her on thyroid hormone replacement. Within six weeks, Karen is back to her old self.
Signs and symptoms of hypothyroidism
Karen illustrates the classic signs and symptoms of hypothyroidism. The signs, including some that Karen did not show, are:
ߜ Slow pulse and enlarged heart
ߜ Enlarged thyroid (goitre), unless prior removal of the thyroid gland is the cause of hypothyroidism