Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (157 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
6.59Mb size Format: txt, pdf, ePub
The patient may present with stigmata of chronic blood loss (
iron deficiency
anemia and related symptoms) or acute blood loss (weakness or syncope).
Screening
: Currently, screening for asymptomatic ulcerated lesions of the GI tract is generally recommended, especially for carcinoma of the colon and large adenomas.
Differential Diagnosis of Upper Gastrointestinal Bleeding (Table
5-3
)
PUD (see discussion of acute abdomen under Abdominal Pain) (40–50% of patients) is associated with risk factors including
H. pylori
infection, use of NSAIDs, stress, and increase of gastric acid. It accounts for gastritis in 10% of patients, esophagitis 6% associated with gastric reflux (GERD). Risk factors for stress-related bleeding include respiratory failure and coagulopathy. Portal hypertension and varices (18% of patients) indicate the severity of a patient’s underlying cirrhosis. These patients have an associated mortality of 50% even after control of the hemorrhage.
Mallory-Weiss tears (5% of patients) occur in the distal esophagus, at the site of the gastroesophageal junction, usually following a bout of retching. Most tears heal uneventfully within 24–48 hours. The diagnosis is made by endoscopic evaluation, at which time therapeutic interventions may be utilized as well as stratifying the risk of rebleeding.
Neoplasm of the esophagus and stomach accounts for <5% of all cases of severe bleeding. It is generally a late manifestation and represents a negative prognostic feature. Uncommonly, tumors may metastasize to the gastric mucosa.
Anticoagulant therapy: GI hemorrhage occurs in 3–4% of patients on anticoagulant therapy; it may be spontaneous or secondary to unsuspected dis-ease (e.g., peptic ulcer, carcinoma, diverticula, hemorrhoids). Occasionally, there is hemorrhage into the wall of the intestine with secondary ileus. PT may be in the therapeutic range or, more commonly, is increased. Warfarin (Coumadin) drug action is potentiated by administration of aspirin, antibiotics, phenylbutazone, and thyroxine and by T-tube drainage of the common bile duct, especially if pancreatic disease is present.
Occult bleeding.
Rendu-Osler-Weber syndrome is associated with telangiectasia of the lips, oral mucosa, and fingertips. Dieulafoy lesion correlates with a dilated aberrant submucosal vessel, which erodes the overlying mucosa in the absence of an ulcer. This should be suspected in the patient with recurrent episodes of undiagnosed upper GI bleeding (GI bleeding in 10–40% of patients).
TABLE 5–3. Differential Diagnosis of Upper Gastrointestinal Bleeding
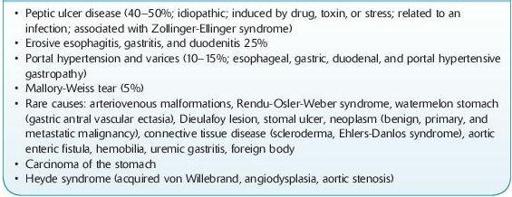
Causes
Mass (e.g., carcinoma, adenoma). In addition to the main cause of bleeding, 50% of patients have an additional lesion that could cause hemorrhage (especially duodenal ulcer, esophageal varices, hiatal hernia). With previously known GI tract lesions, 40% of patients bled from an altogether different lesion.
Inflammation (e.g., IBD, Crohn disease, erosive esophagitis).
Other books
The Dulcimer Boy by Tor Seidler
When We Were Sisters by Emilie Richards
The River of Wind by Kathryn Lasky
Clochemerle by Gabriel Chevallier
Eldritch Manor by Kim Thompson
There's a Man With a Gun Over There by R. M. Ryan
Strangers From the Sky by Margaret Wander Bonanno
Dangerous Love by Walters, Ednah, Walters, E. B.
Hung Out: A Needles and Pins Rock Romance by Creed, Lyrica
Hungry Heart: Konigsburg, Texas, Book 8 by Meg Benjamin