Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (215 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

1. Plasma aldosterone. High plasma aldosterone concentration (PAC) more than 30 ng/dL is suggestive of hyperaldosteronism. Plasma aldosterone concentrations show diurnal variation with highest concentrations at the time of awakening and lowest in the evening. Aldosterone concentrations are related to extracellular fluid volume, being increased by dietary sodium restriction or diuresis and decreased by sodium loading. A rise of plasma aldosterone can occur right after the assumption of upright position. In practice, most centers draw a morning ambulatory upright sample for the assessment of aldosterone and renin levels.
2. Urine aldosterone excretion. Elevated 24-hour urinary aldosterone excretion >15 μg/day is suggestive of hyperaldosteronism.
3. Plasma renin activity (PRA). Plasma renin activity relies on endogenous angiotensinogen in the plasma without addition of angiotensinogen. Renin cleaves angiotensinogen to produce angiotensin I, which can be measured by radioimmunoassay. Plasma renin activity is expressed as the amount of angiotensin I generated per unit of time. Plasma renin activity is low in primary hyperaldosteronism. Conversely, high plasma renin activity can be seen with renovascular or malignant hypertension or secondary to diuretic usage.
4. Plasma aldosterone-to-plasma renin ratio (PAC/PRA ratio). The 2008 Endocrine Society guidelines recommend that the PAC/PRA ratio be used for case detection of primary aldosteronism. Because 30% of the patients with essential hypertension will have low upright renin levels, an elevated plasma aldosterone is required for diagnosis. Hypokalemia must be corrected, and the patient must be off diuretics, angiotensin-converting enzyme (ACE) inhibitors, and high-dose beta-blockers. Primary aldosteronism should be suspected when PRA is suppressed and PAC is increased. Secondary hyperaldosteronism (e.g., renovascular disease) should be considered when both PRA and PAC are increased and the PAC/PRA ratio is <10. An alternate source of mineralocorticoid receptor stimulation such as hypercortisolism or licorice root ingestion should be considered when both PRA and PAC are suppressed.
5. Aldosterone suppression. Oral sodium loading over 3 days is commonly used in many centers. The patients should receive a high-sodium diet for 3 days. The risk of increasing dietary sodium in patients with severe hypertension must be assessed in each case. In addition, because sodium loading typically increases kaliuresis and hypokalemia, serum potassium should be measured daily and vigorous replacement of potassium chloride should be prescribed as indicated. On the 3rd day of the high-sodium diet, serum electrolytes are measured, and a 24-hour urine specimen is collected for the measurement of aldosterone, sodium, and creatinine. The 24-hour urine sodium excretion should exceed 200 meq to document adequate sodium loading. Urine aldosterone excretion 14 μg/day in this setting is consistent with hyperaldosteronism.
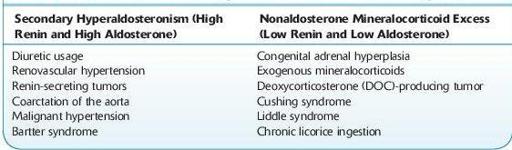
6. Other causes of hypertension with associated hypokalemia need to be ruled out. These include secondary hyperaldosteronism and nonaldosterone mineralocorticoid excess (see Table
6-3
).
7. Patients should be off spironolactone for at least 6 weeks before testing.
8. ACE inhibitors can falsely elevate plasma renin.
9. Patients need to be normokalemic prior to the evaluation of aldosterone because hypokalemia suppresses aldosterone secretion.
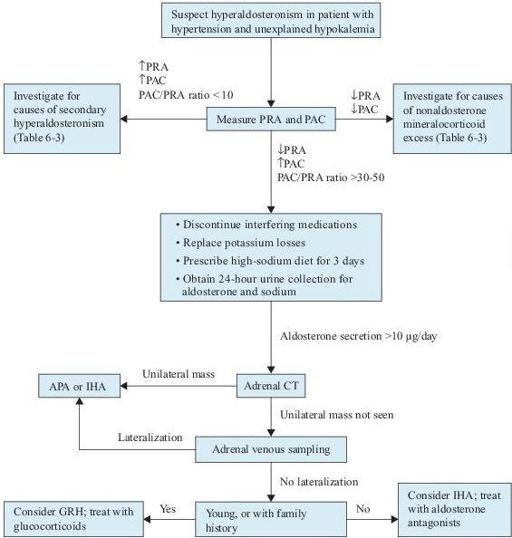
Figure 6–6
Algorithm for the diagnosis of hyperaldosteronism. APA, aldosterone-producing adenoma; CT, computed tomography; GRH, glucocorticoid remediable hyperaldosteronism; IHA, idiopathic hyperaldosteronism; PAC, plasma aldosterone concentration; PRA, plasma renin activity.
TABLE 6–3. Other Causes of Hypertension Associated with Hypokalemia
Imaging Studies
Because of the possibility of “nonfunctioning” adrenal incidentaloma, adrenal image study is recommended after the biochemical analysis indicates the presence of hyperaldosteronism. Once the diagnosis of primary aldosteronism has been established, a unilateral aldosterone-producing adenoma, or rarely carcinoma, must be distinguished from bilateral hyperplasia, since the treatment is different for the two disorders. Adrenal CT is the recommended initial study to determine subtype. CT is helpful in confirming and locating a unilateral mass, such as adenoma or carcinoma. The diagnosis of carcinoma should be suspected when a unilateral adrenal mass is >4 cm in diameter. An abnormality in both glands such as adrenal thickening suggests adrenal hyperplasia. However, patients with hyperplasia may also have normal-appearing adrenal glands on CT.
Additional Study
Adrenal vein sampling can also provide additional information. Measurement of aldosterone in samples of adrenal venous blood, obtained by an experienced radiologist, is the criterion standard test to distinguish between unilateral adenoma and bilateral hyperplasia. Unilateral disease is associated with a marked increase in PAC on the side of the tumor, usually fourfold greater, whereas in patients with bilateral hyperplasia, there is little difference between the two sides.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Stowasser M. Assays of the renin-angiotensin-aldosterone system in adrenal disease. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Young WF, Jr, Kaplan NM, Rose BD. Approach to the patient with hypertension and hypokalemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Young WF, Jr, Kaplan NM, Rose BD. Clinical features of primary aldosteronism. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
ADRENAL MASSES
Definition
Adrenal masses refer to any enlargement of the adrenal glands.
Overview
Adrenal masses can be found in up to 4% of abdominal CT scans done on patients without suspected adrenal problems. The majority of adrenal masses are benign, nonfunctioning adenomas discovered incidentally on abdominal imaging studies (adrenal incidentalomas).
Classification
I. Based on hormonal activity
A. Hormonally active (functional, hypersecretory)
Hypersecreting adrenal adenoma or carcinoma