i bc27f85be50b71b1 (210 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

components that originates from glucose intolerance that in turn
leads to hyperglycemic states (increased plasma glucose levels).
Hyperglycemia can result from insufficient insulin production, ineffective receptive cells for insulin, or both. Insulin promotes storage of glucose as glycogen in muscle tissue and the liver. Deficiency of insulin
leads to increased levels of plasma glucose.I.6,29
The diagnosis of diabetes is based on the presence of any one of the
following three factors6.30:
I . Presence of polyuria, polydipsia, weight loss, blurred vision, and
random plasma glucose (regardless of last meal) greater than or equal
to 200 mgldl



674
AClITE. CARE HANDBOOK FOR PHYSICAL THERAPISTS
2. Fasting plasma glucose greater than or equal to 126 mg/dl (no
caloric intake for at least 8 hours)
3. Two-hour-postload glucose greater than or equal to 200 mgt
dl, using a 75-g oral glucose load dissolved in water
The diagnosis is confirmed when one of the above factors is also
found on a subsequent day.6,3o
The two primary types of diabetes mellitus are type I (insulindependent or juvenile-onset diabetes) and type 2 (non-insulin-dependent Ot adult-onset diabetes). After much debate on the classification of diabetes, the current terminology for diabetes uses type 1 and type
2 diabetes to distinguish between the two primary types.30,JI Orher
forms of glucose intolerance disorders exi t but arc nOt discussed in
this text.
Type 1 Diabetes
Type 1 diabetes is an autoimmune disorder with a genetic-environmental etiology that leads to the selective destruction of beta cells in the pancreas. This destruction results in decreased or absent insulin
secretion. Type 1 diaberes represents 5-10% of the population with
diabetes and generally occurs in individuals under the age of 40
years.29-33 Other etiologies for type I diabetes exist bur arc nOt discussed in this text.
Classic signs and symptoms of type I diabetes are described in the
previous section with the diagnostic criteria for diaberes.6•29
Management of type 1 diabetes may consist of any of the
following.l2-R
o
Close self- or medical monitoring of blood glucose levels (Table
11-8).
•
Insulin administration through oral medications, intramuscular
injection, or continuous subcutaneous insulin infusion (CSII)
pump. CSII therapy has been shown to be as effective as multiple
daily injections of insulin, while also providing the ability to mimic
a more natural glycemic response in fasting and postprandial states
(Table 11-9).
•
Diet modification based on caloric content, proportion of basic
nutrients and optimal sources, and distribution of nutrients in
daily meals.
o
Meal planning.
•
Exercise on a regular basis.

ENDOCRINE SYSTEM
675
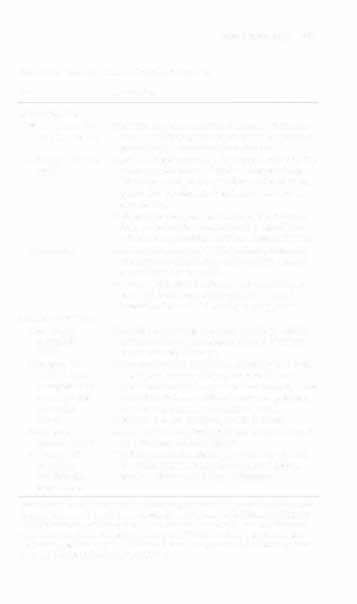
Table 11-8. Tests to Monitor Control of Diabetes
Test
Description
Self-monitoring
Blood glucose fin
Monitors immediate control of diabetes. Very effecger stick samples
tive in establishing the correct insulin dosages and
preventing complications from diabetes.
Reference, 60-110
Capillary blood is obtained by a needle stick of a finmgldl
ger or an earlobe and placed on a reagent strip.
The reagent strip is compared to a color charr or
placed in a porrable electronic meter to read the
glucose level.
Patients in the hospital can also have blood drawn
from an indwelling arterial line, for ease of use,
without compromising accuracy of measurement.
Urine testing
A reagenr strip is dipped in the patienr's urine, and
the strip is compared to a color chart to measure
glucose levels in the urine.
Provides satisfactory results only for patients who
have stable diaberesj otherwise, results can be
insensitive for truly delineating hyperglycemia.
Medical monitoring
Glycosyl.ted
Hyperglycemia results in saturation of hemoglobin
hemoglobin
molecules during the lifespan of a red blood cell
(GHB)
(approximately 120 days).
Reference, 7.5-
Measuring the amount of GHB in the blood provides
11.4% of toral
a weigh red average of the glucose level over a
hemoglobin for
period of time and is a good indicator of long-term
a patient with
control of diabetes, without confounding facrors
controlled
such as a recem meal or insulin injection.
diabetes
Measurements are performed every 3-6 mos.
Fructosamine or
Similar ro GHB test, hyperglycemia saturates serum
glycated protein
proteins, particularly albumin.
Reference, 300
The life span of albumin is approximately 40 days;
mmolliiter
therefore, this test is performed every 3 wks to
=
excellent diamonitor short-term control of diabetes.
betic control
Sources: Data from JV eorbert (ed). Laboratory Tests and Diagnostic Procedures with
Nursing Diagnoses (5th cd). Upper Saddle River, NJ: Prentice Hall Heahh, 2000; 192-
197; LM Malarkey, ME McMorrow (eds), Nurse's Manual of Laboratory Tesrs and
Diagnostic Procedures. Philadelphia: Saunders, 2000;577-580; and RA Sacher, RA
McPherson, JM Campos (eds). Widman's Clinical Interpretation of Laborarory Tests
(II ,h cd). Phil,delphiao D,vis, 2000;817-818.

676
AClJ1'E CARE HANDBOOK FOR PHYSICAL THERAPISTS
Table 11-9. Summary of Insulin Pump T herapy
Patient
Demonstrated ability ro self-monitor glucose Jnd adjust
candidacy
insulin doses based on preprandial blood glucose levels
and anticipated future activity level.
Motivated to achieve and maintain improved glycemic
control using intensive insulin therap}'.
Pregnant padenrs with rype I diabetes.
Patients unaware of hypoglycemic episodes with insulin
therapy.
Patients who experience wide glycemic variations on a
day-co-day basis.
Patients with a significanr rise in hyperglycemia in the
morning ("dawn phenomenon").
Parienrs who need flexibility in their insulin regimen (e.g.,
erratic work schedules, travel frequently).
Adolescents who experience frequent diabetic ketoacidosis.
Night-time usc for children under JO yrs of age who may
nOt be able to adjust their own insulin requirements.
Pump desctiption
Approximately the size of an electronic pager, weighing
only 4 oz.
Padents are instructed on how to insert and change (every
2-3 days) infusion catheters inro rhe subcutaneous
space of their abdomen.
The catheter can be detached from the insulin pump for
bathing or intimate cooract.
Two serrings: basal rate and bolus doses, borh adjustable
by rhe patient depending on needs (e.g., preprandial
boilis or decreased basal rate with exercise).
Battery life is approximately 6 wks.
Types of insulin
Regular human buffered insulin (shorr acting).
Insulin analog (rapid acting).
Pump
Hyperglycemia and diabetic keroacidosis.
complications
Hypoglycemia and hypoglycemic unawareness.
Skin infections.
Weighr gain.
Sources: Data from J Unger. A primary care approach [0 continuous subcutaneous insulin infusion. Clin Diaberes 1999; 17(3): I 13; Conrinuous subcmancolls insulin. Diabetes Carc 2001 ;24( 1 ):598; and FR Kaufman, M Halvorson, C Kim, P Pitukcheew:mollt. Use