i bc27f85be50b71b1 (30 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

•
An example of a disproportionate HR response to low-level
activity (bed or seared exercises or ambulation in room) is an HR
of more than 120 bpm or less rhan 50 bpm H
• When prescribing activity intensity for a patient taking betablockers, the HR should not exceed 20 beats above resting HR.
• If prescribing activity intensity using HR for patients with an
A1CD, the exercise target HR should be 20-30 beats below the
threshold rate on the defibrillator.52
•
H R cannot be lIsed to prescribe exercise starus post heart transplant secondary to denervation of the heart during transplantation.
•
Baseline HR and recent changes in medications should always
be considered before beginning an exercise session.
2.
BP: Refer to the cardiac assessment section regarding BP mea-
surements and Table 1-6 for BP ranges. Examples of a disproportionate
response to exercise are a systolic pressure decrease of 10 mm Hg below
the resting value, a hypertensive systolic response of more than 1 80 mm
Hg, or a hypertensive diastolic response of more than 1 1 0 mm Hg."
• If the patient is on a pacemaker that does nor have rare modulation, BP response can be used to gauge intensity. Please refer to the Procedures section for the discussion on pacemakers.

CARDIAC SYSTEM
67
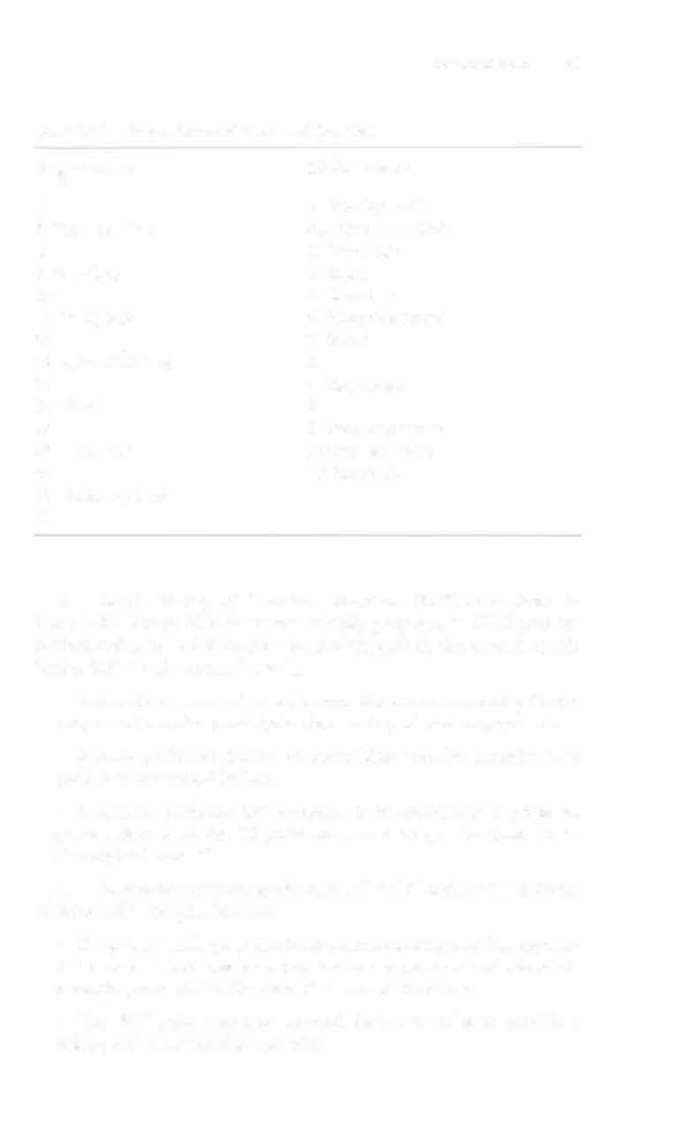
Table 1-22. Borg's Rating of Perceived Exertion
Original Scale
I O-Point Scale
6
o Nothing at all
7 Very, very Iighr
0.5 Very, very slight
8
1 Very slight
9 Very light
2 Slight
1 0
3 Moderare
1 1 Fairly light
4 Somewhar severe
12
5 Severe
13 Somewhar hard
6
14
7 Very severe
15 Hard
8
1 6
9 Very, very severe
17 Very hard
(almost maximal)
1 8
1 0 Maximal
19 Very, very hard
20
3.
Borg's Rating of Perceived Exertioll (RPE) is depicted in
Table ] -22. Borg's RPE scale was initially proposed in 1 962 and has
evolved today to be the classic means of objectively documenting subjective feelings of exercise intensity.
• This scale can be easily used to monitor exercise intensity for the
purpose of exercise prescription in a variety of patient populations.
• It is the preferred method of prescribing exercise intensity for a
patient taking beta-blockers.
• A general guideline for everyone is to exercise to a point no
greater than 5 on the 1 0-point scale and no greater than 1 3 on
the original scale.52
4.
Rate pressure product (RPP) is HR x SBP and is an indication
of myocardial oxygen demand.
• If a patient undergoes maximal exercise testing and has myocardial ischemia, RPP can be calculated at the point when ischemia is occurring to establish the patient'S ischemic threshold.
• This RPP value can then be used during exercise to provide a
safe guideline of exercise intensity.
68 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
5.
Heart sounds: Refer to the section on Auscultation and Table
1-9 for normal and abnormal heart sounds.
• The onset of murmurs, S3 heart sounds, or S4 heart sounds during treatment may be detected and could indicate a decline in cardiac function during activity. This finding should be brought to the attention of the nurse and physician.
6.
Breath soul/ds: Refer to Chapter 2 for a discussion of lung
auscultation and the interpretation of breath sounds.
• The presence of or increase in bibasilar crackles during activity
may be indicative of acute CHE Activity should be terminated and
the nurse and physician notified.
7.
fCC rhythm: Refer to the section on ECC and the section
Rhythm and Conduction Disturbance.
•
When treating pacients who are being continuously monirored
by an ECC, it is important to know their baseline rhythm, the most
recently observed rhythm, what lead is being monitored, and why
they are being monitored.
•
It is important to recognize their normal rhythm and any deviations from this norm. It is also important ro recognize changes that could indicate a decline in cardiac status. Examples of declining
cardiac status include the following:
•
Onset of ST changes (elevation or depression of more than 1
mm) could indicate ischemia
•
Increased frequency of PVCs (trigeminy to bigeminy or couplets)
•
Unifocal PVCs to multifocal PVCs
• Premature atrial contractions to atrial flutter or atrial fibrillation
• Atrial flutter to atrial fibrillation
• Any progression in heart blocks (first degree to Mobitz I)
• Loss of pacer spike capturing (pacer spike without resultant
QRS complex on ECC)
• The physical therapist should also be able to recognize signs and
symptoms of cardiac decompensation and immediately notify the
physician if any develop (see Figure 1 - 1 0). It is important to record
any signs noted during activity and other objective data at that


CARDIAC SYSTF�1
69
time. Other signs and symptoms include weakness, fatigue, dizziness, lightheadedness, angina, palpitations, and dyspnea. It is important to record any symptoms reported by the patient and any
objective information at that time (ECG readings; SP, HR, and
RPP measurements; breath sounds).
Clinical Tip
Patients should be encouraged to report any symptom(s),
even if they think it is trivial.
References
I. American Heart Association. 2001 Heart and Stroke Statistical Update.
Dallas: American Heart Association, 2000.
2. Moore K (cd). Clinically Oriented Anatomy (3rd ed). Baltimore: Williams & Wilkins, 1 992.
3. Guyton AC (ed). Textbook of Medical Physiology (9th ed). Philadelphia: Saunders, 1 996.
4. Cheitlin MD, Sokolow M, McUroy MB (eds). Clinical Cardiology (6th
ed). Norwalk, CT: Appleton & Lange, 1 993.
5. Braunwald E (cd). Heart Disease: A Textbook of Cardiovascular Medicine (4th cd). Philadelphia: Saunders, 1 992.
6. Davis D (ed). How co Quickly and Accurately Master ECG Interpretation (2nd cd). Philadelphia: Lippincott, 1992.
7. Hillis LD, Firth BG, Willerson JT (eds). Manual of Clinical Problems in
Cardiology. Boston: Liede, Brown, 1 984.
8. Task Force of the European Sociery of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use.
Circulation 1 996;93: 1 043-1 065.
9. Bernsron G, Cacioppo JT, Quigley KS. Autonomic determinism: the
modes of autonomic control, the doctrine of autonomic space, and the
laws of auronomic constraint. Psychol Rev 1 99 1 ;98:459-487.
1 0. Urden LD, Davie JK, Thelan LA (eds). Essentials of Critical Care Nursing. St. Louis: Mosby, 1992.
I I . Cohen M, Michel TH (eds). Cardiopulmonary Symptoms in Physical
Therapy Practice. New York: Churchill Livingsrone, 1 988.
1 2. Woods SL, Sivarajian Froelicher ES, Underhill-Motzer S (eds). Cardiac
Nursing (4th ed). Philadelphia: Lippincorr, 2000.
