Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (3 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.65Mb size Format: txt, pdf, ePub
Prolonged QT interval (
NEJM
2008;358:169;
www.torsades.org
)
• QT measured from beginning of QRS complex to end of T wave (measure longest QT)
• QT varies w/ HR → correct w/ Bazett formula: QTc = QT/√RR (in sec), formula inaccurate at very high and low HR (nl QTc <440 msecand <460 msec
)
• QT prolongation a/w ↑ risk TdP (esp. >500 msec); perform baseline/serial ECGs if using QT prolonging meds, no estab guidelines for stopping Rx if QT prolongs
• Etiologies:
Antiarrhythmics
: class Ia (procainamide, disopyramide), class III (amiodarone, sotalol)
Psych drugs
: antipsychotics (phenothiazines, haloperidol, atypicals), Li, ? SSRI, TCA
Antimicrobials
: macrolides, quinolones, azoles, pentamidine, atovaquone, atazanavir
Other
: antiemetics (droperidol, 5-HT
3
antagonists), alfuzosin, methadone, ranolazine
Electrolyte disturbances
: hypoCa (nb, hyperCa a/w ↓ QT), ? hypoK, ? hypoMg
Autonomic dysfxn
: ICH (deep TWI), stroke, carotid endarterectomy, neck dissection
Congenital
(long QT syndrome): K, Na, Ca channelopathies (
Circ
2013;127:126)
Misc
: CAD, CMP, bradycardia, high-grade AVB, hypothyroidism, hypothermia, BBB
Left ventricular hypertrophy (LVH) (
Circ
2009;119:e251)
• Etiologies: HTN, AS/AI, HCMP, coarctation of aorta
• Criteria (all w/ Se <50%, Sp >85%; accuracy affected by age, sex, race, BMI)
Romhilt-Estes point-score system: 4 points = probable, 5 points = definite ↑ Amplitude (any of the following): largest R or S in limb leads ≥20 mm
or
S in V
1
or V
2
≥30 mm
or
R in V
5
or V
6
≥30 mm (3 points)
ST displacement opposite to QRS deflection: w/o dig (3 points); w/ dig (1 point)
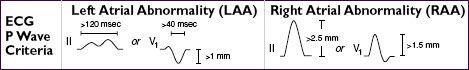
LAA (3 points); LAD (2 points); QRS duration ≥90 msec (1 point)
Intrinsicoid deflection (QRS onset to peak of R) in V
5
or V
6
≥50 msec (1 point)
Sokolow-Lyon: S in V
1
+ R in V
5
or V
6
≥35 mm or R in aVL ≥11 mm
Cornell: R in aVL + S in V
3
>28 mm in men or >20 mm in women
If LAD/LAFB, S in III + max (R+S) in precordium ≥30 mm
Right ventricular hypertrophy (RVH) (
Circ
2009;119:e251)
• Etiologies: cor pulmonale, congenital (tetralogy, TGA, PS, ASD, VSD), MS, TR
• Criteria (all tend to be insensitive, but highly specific, except in COPD)
R > S in V
1
or R in V
1
≥7 mm, S in V
5
or V
6
≥7 mm, drop in R/S ratio across precordium
RAD ≥ +110° (LVH + RAD
or
prominent S in V
5
or V
6
→
biventricular
hypertrophy)
Ddx of dominant R wave in V1 or V2
• Ventricular enlargement: RVH (RAD, RAA, deep S waves in I, V
5
, V
6
); HCMP
• Myocardial injury: posterior MI (anterior Rw = posterior Qw; often with IMI)
• Abnormal depolarization: RBBB (QRS >120 msec, rSR′); WPW (↓ PR, Δ wave, ↑ QRS)
• Other: dextroversion; Duchenne muscular dystrophy; lead misplacement; nl variant
Poor R wave progression (PRWP) (
Am Heart J
2004;148:80)
• Definition: loss of anterior forces w/o frank Q waves (V
1
–V
3
); R wave in V
3
≤3 mm
• Possible etiologies (nonspecific):
old anteroseptal MI (usually w/ R wave V
3
≤1.5 mm, ± persistent ST ↑ or TWI V
2
& V
3
) cardiomyopathy
LVH (delayed RWP with prominent left precordial voltage), RVH, COPD (which may also have RAA, RAD, limb lead QRS amplitude ≤5, S
I
S
II
S
III
w/ R/S ratio <1 in those leads)
LBBB; WPW; clockwise rotation of the heart; lead misplacement; PTX
Pathologic Q waves
• Definition: ≥30 msec (≥20 msec V
2
–V
3
) or >25% height of R wave in that QRS complex
• Small (septal) q waves in I, aVL, V
5
& V
6
are nl, as can be isolated Qw in III, aVR, V
1
• “Pseudoinfarct” pattern may be seen in LBBB, infiltrative dis., HCMP, COPD, PTX, WPW
ST elevation (STE) (
NEJM
2003;349:2128;
Circ
2009;119:e241 & e262)
•
Acute MI
(upward convexity ± TWI) or prior MI with persistent STE
•
Coronary spasm
(Prinzmetal’s angina; transient STE in a coronary distribution)
•
Myopericarditis
(diffuse, upward concavity STE; a/w PR ↓; Tw usually upright)
•
HCMP
,
Takotsubo CMP
,
ventricular aneurysm
, cardiac contusion
•
Pulmonary embolism
(occ. STE V
1
–V
3
; typically associated TWI V
1
–V
4
, RAD, RBBB)
•
Repolarization abnormalities
LBBB (↑ QRS duration, STE discordant from QRS complex)
dx of STEMI in setting of LBBB: ≥1 mm STE concordant w/ QRS (Se 73%, Sp 92%), STD ≥1 mm V
1
–V
3
(Se 25%, Sp 96%) or STE ≥5 mm discordant w/ QRS (Se 31%, Sp 92%) (“Sgarbossa criteria,”
NEJM
1996;334:481)
LVH (↑ QRS amplitude); Brugada syndrome (rSR′, downsloping STE V
1
–V
2
)
Hyperkalemia (↑ QRS duration, tall Ts, no Ps)
•
aVR
: STE >1 mm a/w ↑ mort in STEMI; STE aVR > V
1
a/w left main disease
•
Early repolarization
: most often seen in V
2
–V
5
& in young adults (
Ann Emerg Med
2012;60:45)
J point ↑ 1–4 mm; notch in downstroke of R wave; upward concavity of ST; large Tw;
ratio of STE / T wave amplitude <25%; pattern may disappear with exercise
? early repol in inf leads may be a/w ↑ risk of VF (
NEJM
2009;361:2529;
Circ
2011;124:2208)
ST depression (STD)
•
Myocardial ischemia
(± Tw abnl) or acute true posterior MI (V
1
–V
3
)
• Digitalis effect (downsloping ST ± Tw abnl, does
not
correlate w/ dig levels)
• Hypokalemia (± U wave)
• Repolarization abnl in a/w LBBB or LVH (usually in leads V
5
, V
6
, I, aVL)
T wave inversion (TWI; generally ≥1 mm; deep if ≥5 mm) (
Circ
2009;119:e241)
• Ischemia or infarct; Wellens’ sign (deep early precordial TWI) → proximal LCA lesion
• Myopericarditis; CMP (Takotsubo, ARVC, apical HCM); MVP; PE (esp. if TWI V
1
–V
4
)
• Repolarization abnl in a/w LVH/RVH (“strain pattern”), BBB
• Posttachycardia or postpacing
• Electrolyte, digoxin, PaO
2
, PaCO
2
, pH or core temperature disturbances
Other books
The Day to Remember by Jessica Wood
Reckless Heat: A Hostile Operations Team Prequel by Lynn Raye Harris
Atonement by J. H. Cardwell
Sweet Charity by Sherri Crowder
Earth Unaware (First Formic War) by Card, Orson Scott, Johnston, Aaron
The Burglar Who Thought He Was Bogart by Lawrence Block
2#Awakened by the Vampire Prince (Flower) by Hartnady, Charlene
Just for Now by Abbi Glines
Objetivo 4 by German Castro Caycedo
Turn of the Moon (A Royal Shifters novel Book 1) by Dover, L.P.