Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (6 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
8.04Mb size Format: txt, pdf, ePub
•
Cardiac biomarkers
(Tn preferred, or CK-MB): ✓ Tn at baseline & 3–6 h after sx onset; a rise to >99th %ile in approp. clinical setting dx of MI (see “Chest Pain”); nb, in Pts w/ ACS & ↓ CrCl, ↑ Tn still portends poor prognosis (
NEJM
2002;346:2047) • If low prob,
stress test
,
CT angio
or rest perfusion imaging to r/o CAD (see “Chest Pain”) • TTE (new wall motion abnl) suggestive of ACS; coronary angio gold standard for CAD
Prinzmetal’s (variant) angina
• Coronary spasm → transient STE usually w/o MI (
but
MI, AVB, VT can occur) • Pts usually young, smokers, ± other vasospastic disorders (eg, migraines, Raynaud’s) • Angiography → nonobstructive CAD, focal spasm w/ hyperventilation, acetylcholine • Treatment: high-dose CCB, nitrates (+SL NTG prn), ? a-blockers; d/c smoking • Cocaine-induced vasospasm: use CCB, nitrates, ASA; ? avoid bB, but data weak and labetalol appears safe (
Archives
2010;170:874;
Circ
2011;123:2022)
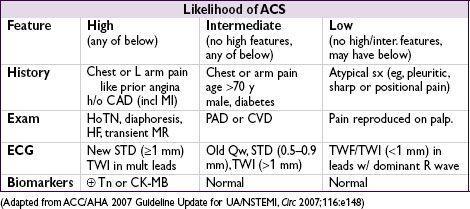
Approach to triage
• If hx and initial ECG & biomarkers non-dx, repeat ECG & biomarkers 3–6 h later • If remain nl and low likelihood of ACS, search for alternative causes of chest pain • If remain nl, have ruled out MI,
but
if suspicion for ACS based on hx, then still need to r/o UA w/ stress test to assess for inducible ischemia (or CTA to r/o CAD);
if low risk (age ≤70; prior CAD, CVD, PAD; rest angina) can do as outPt w/in 72 h (0% mortality, <0.5% MI,
Ann Emerg Med
2006;47:427)
if not low risk, admit and initiate Rx for possible ACS and consider stress test or cath
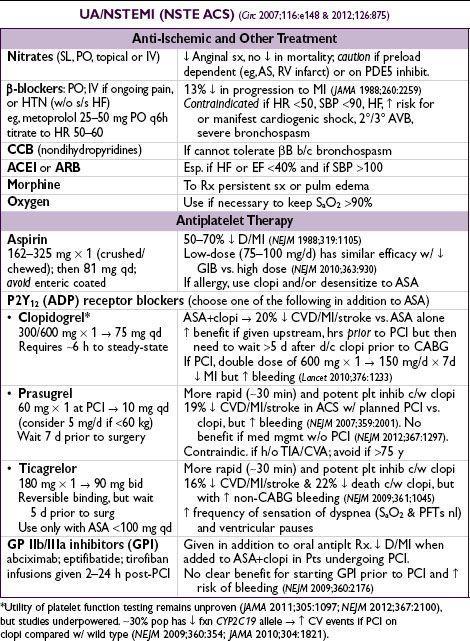
Coronary angiography (
Circ
2007;116:e148 & 2012;126:875)
•
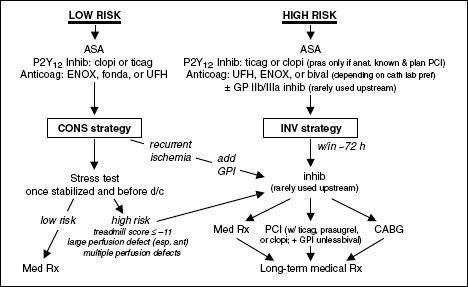
Conservative strategy
= selective angiography. Medical Rx with pre-d/c stress test; angio only if recurrent ischemia or stronglyETT.
Indicated for
: low TIMI risk score, Pt or physician preference in absence of high-risk features, low-risk women (
JAMA
2008;300:71).
•
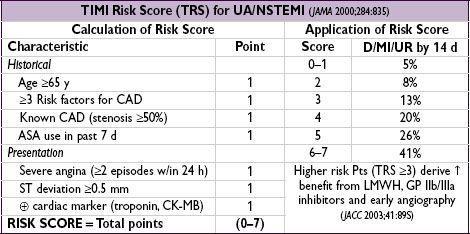
Invasive strategy
= routine angiography w/in 72 h
Immediate (w/in 2 h) if
: refractory/recurrent ischemia, hemodynamic or electrical instability
Early (w/in 24 h) if
:Tn, ST Δ, TRS ≥3, GRACE risk score >140 (
NEJM
2009;360:2165)
Delayed (ie, acceptable anytime w/in 72 h) if
: diabetes, EF <40%, GFR <60, post-MI angina, PCI w/in 6 mo, prior CABG or high-risk stress results
32% ↓ rehosp for ACS, nonsignif 16% ↓ MI, no Δ in mortality c/w cons. (
JAMA
2008;300:71)
↑ peri-PCI MI counterbalanced by ↓↓ in spont. MI
Mortality benefit seen in some studies, likely only if cons. strategy w/ low rate of angio
Figure 1-2
Approach to UA/NSTEMI
STEMI
Requisite STE (at J point)
• ≥2 contiguous leads w/ ≥1 mm (except for V
2
–V
3
: ≥2 mm inand ≥1.5 mm in
) • New or presumed new LBBB
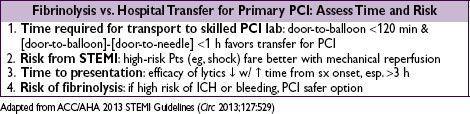
Reperfusion (“time is muscle”)
• Immediate reperfusion (ie, opening occluded culprit coronary artery) is critical • In PCI-capable hospital, goal should be
primary PCI
w/in 90 min of 1st medical contact • In non-PCI-capable hospital, consider
transfer
to PCI-capable hospital (see below), o/w
fibrinolytic therapy
w/in 30 min of hospital presentation • Do not let decision regarding
method
of reperfusion delay
time
to reperfusion
Primary PCI (
NEJM
2007;356:47)
• Indic: STE + sx <12 h; ongoing ischemia 12–24 h after sx onset; shock regardless of time • Superior to lysis: 27% ↓ death, 65% ↓ reMI, 54% ↓ stroke, 95% ↓ ICH (
Lancet
2003;361:13) • Thrombus aspiration during angio prior to stenting ↓ mortality (
Lancet
2008;371:1915) • Do not intervene on nonculprit lesions; risk stratify w/ imaging stress (
Circ
2011;124:e574) •
Transfer
to center for 1° PCI may also be superior to lysis (
NEJM
2003;349:733), see below
Other books
Cynthia Bailey Pratt by Gentlemans Folly
A Commitment to Love, Book 3 by Kenya Wright
Falling On the Sword by Alex Ankrom
Lucky Horse by Bonnie Bryant
Finding the Wolf(The Dragon's Hoard #1) by Mell Eight
Bethany Caleb by Spofford, Kate
Cuffed by A Muse
Lowland Rider by Chet Williamson
El sueño robado by Alexandra Marínina
Motherland by William Nicholson