Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine
The Washington Manual Internship Survival Guide (5 page)

WORKING WITH DIFFICULT PATIENTS
•
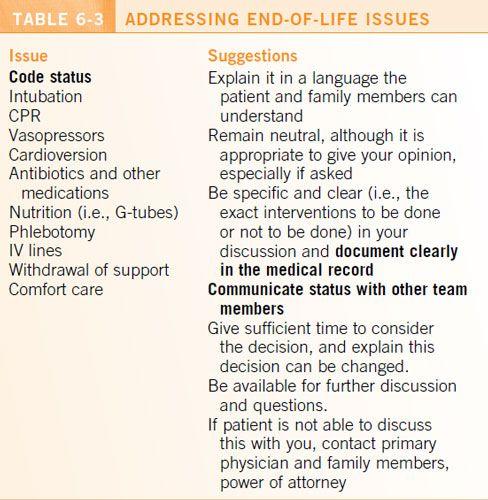
Be proactive and address potential concerns, expectations, or questions upfront (see
Tables 6-2
and
6-3
). Checking in with the patient at regular intervals builds rapport and can save you from multiple phone calls. Try to minimize waiting time and interruptions during meetings.
•
Be as flexible and as accommodating as you can. Recognize that the patient may be tired of repeating his or her history or having a physical examination.
•
Let the patient (and loved ones) know about the management plan at least once a day. Inform him or her of the test results and changes in the plan, and let him or her know if consultants will be coming by.
•
Avoid promises that you cannot fulfill. This includes the time of discharge or the time of a diagnostic procedure.
•
If more than one service is involved, designate someone to be the primary source of communication to avoid confusion.
•
The patient’s “difficult” behavior may stem from lack of control over decision making and the situation or lack of insight into his or her medical condition. Past experiences, things the patient may have seen or read in the media, and fear may also play a role. Active listening, acknowledging the patient’s point of view, and reassurance can go a long way.
•
Acknowledge your own frustration, seek the advice of others when necessary, and always try to do what’s best for the patient.



Patient Safety
7
Patient safety is a priority for all entities of patient care from physicians, to nurses, to ancillary staff. The most important advice an intern can follow concerning patient safety is to feel comfortable in your decision making, and if you don’t feel comfortable, seek help from your upper-level residents or attending physician. A little bit of caution and mindfulness can prevent unnecessary errors and potential patient harm.
MOST COMMON MEDICAL ERRORS
•
Medication errors
• These are the errors most commonly encountered on the ward and also the most avoidable. The most common medication errors include missed doses, wrong dosages, infusion errors, patient allergy, and orders entered on the wrong patient.
• When discharging patients, it is important to ensure that all medications are reconciled, prescriptions are correctly filled out, and the patient has adequate instructions for use.
•
Procedure-related errors
• Be sure to obtain proper informed consent.
• The most common errors encountered during procedures include incorrect patient/site, failure to review labs, line infections, incorrect documentation, and periprocedural adverse events. You should always review pertinent labs/imaging, including platelet count, and INR prior to every procedure to reduce bleeding risk.
• A “time out” should be done before all but trivial procedures.
• Central line–associated bloodstream infections are an unfortunate complication of procedures, but they can be minimized with sterile technique and adequate preparation.
• Residents are always available to help/supervise any procedures that you are not comfortable with.
•
Ancillary staff communication
• An integral part of any admission is open and continued communication with all participants of patient care.
• Be sure to set a comfortable climate in which other healthcare providers can express their opinions and concerns.
•
Prophylactic measures
• Should the patient be in some form of isolation?
• Does the patient need DVT/PE prophylaxis?
• Are fall precautions indicated?
• Is the patient at risk for delirium and/or substance withdrawal?
• Are there unnecessary lines (e.g., bladder catheters, peripheral IVs, peripherally inserted central lines, central lines) that are sources of potential infection?
ERROR DISCLOSURE
Errors are bound to occur, and expedient identification, correction, and disclosure will prevent further escalation. It is important to disclose medical error/mistakes and explain how the error occurred and what you plan to do to correct the error. Studies have shown that patients are more receptive to open admittance of errors than to attempts at concealment. Medical errors must also be relayed to not only your supervising resident but also charge nurses on the floor and your institution’s risk management department.
Risk Management
8
•
The goal of risk management is to improve the quality of patient care and reduce the liability to the healthcare provider.
•
Physicians are obligated to inform patients when there is an adverse event, even if the patient was not noticeably harmed.
•
Disclosing adverse events should be done with the help of your attending physician and risk management (see
Table 8-1
). Reporting adverse events not only is important to patient care but also helps identify major system flaws.
DEFINITIONS
•
Adverse event:
any incident, therapeutic error, iatrogenic injury, or other undesirable occurrence that caused probable or definite harm to a patient.
•
Disclosure of adverse events:
an honest and empathetic discussion of clinically significant facts between providers and the patient about the occurrence of an adverse event that resulted or could have resulted in patient harm.
•
Sentinel event:
unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Requires immediate investigation and response.
HOW TO RESPOND TO A POTENTIAL INCIDENT
•
Arrive as soon as possible.
•
Avoid assigning blame to an individual.
•
Never argue in public or in the chart.
•
Document the facts.
•
Report injuries.
•
Never state in the medical record that an incident report was completed.

HOW TO REPORT AN ERROR
•
Call risk management at your institution.
•
Complete an incident report.
•
Discuss the situation with your resident and attending as soon as possible (see
Table 8-1
).
HOW TO DISCLOSE AN ADVERSE EVENT
•
Speak with your resident, attending physician, and risk management first.
•
Your attending should coordinate disclosure efforts and speak with the patient and family.
•
If more than one service is involved, confer and collaborate on the disclosure conversation. The medical care team should deliver a consistent message.
•
Give the patient and family an honest, straightforward, and prompt explanation of what occurred.
•
You can apologize for the error.
•
If the cause of error is uncertain, do not speculate or hypothesize. State the facts. Tell the patient that further investigation is necessary.
•
Identify who will be involved with ongoing care. You may need to transfer the patient’s care if the patient–physician relationship has been compromised.
•
Tell the patient and family what steps are being undertaken to prevent further error.
•
Allow time for questions.
•
Speak in layman’s terms.
•
Be aware of body language.
•
Document the discussion with the family
• Time, date, and place
• Names and relationships of those present
• Documentation of discussion of event
• Patient/family response
DOCUMENTATION
•
Documentation is vitally important whenever there has been an adverse event.
•
Prior to writing a note, give yourself a few minutes to recap what happened. Remember: “If it wasn’t documented, it wasn’t done.”
Do
•
Record changes in patient’s condition and response to treatment.
•
Add addendums when necessary.
•
Write legibly.
•
Use factual and objective language.
