Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (207 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
12.23Mb size Format: txt, pdf, ePub
1. Classic symptoms of hyperglycemia, such as thirst, polyuria, weight loss, visual blurring
2. Serendipitous finding of hyperglycemia or known impaired glucose tolerance
3. Complications of diabetes, such as proteinuria, neuropathy, cardiovascular complications, and retinopathy
4. Evidence of dehydration, orthostatic hypotension, confusion, or coma
Screening for Diabetes Mellitus
A. In the absence of specific symptoms
Routine screening for type 1 DM is not recommended, since there is no accepted treatment for the asymptomatic phase of type 1 DM.
However, for type 2 DM, the American Diabetes Association (ADA) recommends screening for diabetes or prediabetes in all adults with body mass index (BMI) ≥25 kg/m
2
and one or more additional risk factors for diabetes (see subsequent text of this Chapter). In individuals without risk factors, testing should begin at age 45 years. Fasting plasma glucose is the recommended screening test, since it is faster, easier to perform, more convenient, acceptable to patients, and less expensive.
B. Risk factors for diabetes
1. Age ≥45 years
2. Overweight (body mass index ≥25 kg/m
2
)
3. Family history diabetes mellitus in a first-degree relative
4. Habitual physical inactivity
5. Belonging to a high-risk ethnic or racial group (e.g., African American, Hispanic, Native American, Asian American, and Pacific Islander)
6. History of delivering a baby weighing >4.1 kg (9 lb) or of gestational DM
7. Hypertension (blood pressure ≥140/90 mm Hg)
8. Dyslipidemia defined as a serum high-density lipoprotein cholesterol concentration ≤35 mg/dL (0.9 mM) and/or a serum triglyceride concentration ≥250 mg/dL (2.8 mM)
9. Previously identified impaired glucose tolerance (IGT) or impaired fasting glucose (IFG)
10. Polycystic ovary syndrome
11. History of vascular disease
How to Confirm the Diagnosis
ADA Criteria for the diagnosis of diabetes mellitus:
a. Symptoms of diabetes and a casual plasma glucose ≥200 mg/dL (11.1 mM). Casual is defined as any time of day without regard to time since the last meal. The classic symptoms of diabetes include polyuria, polydipsia, and unexplained weight loss.
Or
b. Fasting plasma glucose ≥126 mg/dL (7.0 mM). Fasting is defined as no caloric intake for at least 8 hours.
Or
c. Two-hour plasma glucose ≥200 mg/dL (11.1 mM) during an oral glucose tolerance test (OGTT). The test should be performed using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.
Or
d. Glycosylated hemoglobin A1c (HbA
1c
) ≥6.5%. In 2010, the ADA added this as another criterion for the diagnosis of DM. The diagnostic test should be performed using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized or traceable to the Diabetes Control and Complications Trial reference assay. Point-of-care HbA
1c
assays are not sufficiently accurate at this time to use for diagnostic purposes. HbA
1c
is an extremely valuable clinical tool useful both in the diagnosis and in management of diabetic patients. HbA
1c
has a circulating life span of about 90 days, and thus the measurement of HbA
1c
provides information about the level of glycemic control over a 3-month period. However, if the patient’s red blood cells have abnormal survival time, the value of HbA
1c
may not be reliable. It will be falsely low in patients with hemolytic anemias, and it may be falsely elevated in patients with polycythemia vera or postsplenectomy. It cannot be used as a reliable index for glycemic control in patients with chronic liver diseases due to increased erythrocyte turnover.
In the absence of unequivocal hyperglycemia, the diagnosis of DM must be confirmed on a subsequent day by measuring any one of the three criteria (b, c, and d). However, in symptomatic patients with blood glucose ≥200 mg/dL (11.1 mM) or patients with ketonuria and clear manifestations of type 1 DM, the diagnosis is established and further evaluation is not needed.
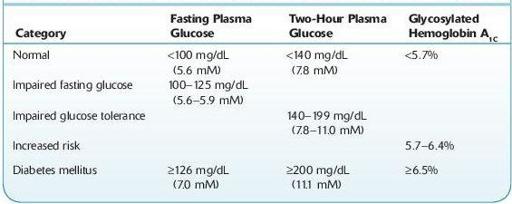
Patients with prediabetic conditions (Table
6-1
) should be counseled on issues related to lowering their risk for macrovascular diseases (smoking cessation, use of aspirin, diet, and exercise), should have measurements of blood pressure and serum lipids, and should also be encouraged to modify their lifestyle and reduce their weight.
TABLE 6–1. Diagnostic Thresholds for Diabetes and Prediabetic Conditions
Complications
Evaluation for complications of diabetes should be done routinely in diabetic patients.
A. Routine eye examination
B. Routine foot examination
C. Screening for microalbuminuria
D. Screening for coronary heart disease
Acute Complications
Excessive and prolonged hyperglycemia associated with uncontrolled diabetes can cause fluid and electrolyte imbalance, which may be life-threatening.
A.
Diabetic ketoacidosis
(mostly in type 1 DM, may also be seen in type 2 DM): Absolute insulin deficiency leads to the unopposed action of the counterregulatory hormones, including glucagon on the liver, adipose tissue, and muscle, leading to unchecked gluconeogenesis and lipolysis.
a.
Signs and symptoms
1. Dehydration, fruity breath smell, orthostatic hypotension, tachypnea, tachycardia, abdominal pain, nausea, vomiting, and confusion
2. Antecedent history of viral or bacterial illness, trauma, or emotional stress
b.
Laboratory findings
1. Hyperglycemia (generally ≥300 mg/dL), glucosuria, ketonemia and ketonuria, low bicarbonate, elevated blood urea nitrogen, elevated creatinine, pH usually <7.3.
2. Decreased total body potassium and phosphorus. Serum levels may be normal due to acidosis and shifts to the extracellular space.
B.
Hyperosmolar hyperglycemic nonketotic coma:
Hyperglycemia in patients with type 2 DM can lead to hyperosmolar coma. The degree of hyperglycemia and dehydration that develop is often far more severe than in patients with type 1 DM.
a.
Signs and symptoms
1. Usually occurs in elderly patients with decreased ability to obtain free water; precipitated by illness or drugs
2. Deceased mentation, coma
3. Dehydration
b.
Laboratory findings
1. Hyperglycemia (glucose often ≥600 mg/dL)
2. Serum osmolarity often ≥320 mOsm/kg
3. Bicarbonate remains ≥15 mEq/L
4. pH remains ≥7.3
Chronic Complications
A. Microvasculopathy
a. Diabetic nephropathy
1. Diabetes is now the most common cause of end-stage renal disease in Western countries.
2. Twenty to thirty percent of patients with diabetes will develop evidence of nephropathy.
3. The earliest evidence of nephropathy is the appearance of low levels of albumin (30 mg/day or 20 μg/minute) in the urine, termed microalbuminuria.
4. Eighty percent of type 1 DM and 20–40% of type 2 DM patients who develop microalbuminuria will progress to overt nephropathy (≥300 mg/ day or 200 μg/minute) over a period of 10–15 years if not treated.
5. Of those patients who develop overt nephropathy, end-stage renal disease can be expected to develop in 75% of patients with type 1 DM and 20% of patients with type 2 DM over 20 years.
b. Retinopathy and neuropathy
B. Macrovasculopathy and vascular atherosclerosis are also major complications of DM.
Suggested Readings
Khan F, Sachs H, Pechet L.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Other books
The Silent Twin by Unknown
The Unfinished Song (Book 5): Wing by Tara Maya
He Runs (Part One) by Seth, Owen
Not Just a Witch by Eva Ibbotson
Mine by Brett Battles
The Angel Singers by Dorien Grey
The Worst of Me by Kate Le Vann
Caitlyn and the Alien Protector (Intergalactic Brides 7) by Jessica Coulter Smith
The 30 Day MBA by Colin Barrow
Shackled by the Dictator (BDSM Erotica) by Aphrodite Hunt