Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (229 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

The main goal of hypercalcemia workup is to differentiate PTH-mediated hypercalcemia from non–PTH-mediated hypercalcemia.
Interpretation of serum calcium. Approximately 40–50% protein bound (predominantly to albumin), but only the ionized or free of the circulating calcium concentration is physiologically important. Hypercalcemia is caused by an elevation in the ionized or free calcium concentration. In patients with hypo- or hyperalbuminemia, the measured calcium concentration should be corrected for abnormality in albumin. Pseudohypercalcemia should be excluded; it is related to increased protein binding due to either severe dehydration and hyperalbuminemia or production of calciumbinding paraprotein in patients with multiple myeloma. On the contrary, in patients with hypoalbuminemia due to chronic illness or malnutrition, total serum calcium concentration may be normal when serum ionized calcium is elevated.
Calcium results need to be repeated if abnormal. A single elevated serum calcium concentration should be repeated to confirm the diagnosis.
Serum calcium should not be measured after a recent high-calcium meal.
A 24-hour urine calcium quantification is useful in differentiating primary hyperparathyroidism from familial hypocalciuric hypercalcemia (FHH).
PTH. Measurement of intact PTH via immunoradiometric assays is the current standard for the diagnosis of hyperparathyroidism. PTH will be elevated in 80–90% of patients with primary hyperparathyroidism.
Parathyroid hormone–related protein (PTHrP). In the presence of hypercalcemia, if PTH level is appropriately suppressed, then evaluation for other causes should include the measurement of PTHrP. PTHrP is the most common tumor product implicated in the hypercalcemia of malignancy.
Vitamin D metabolites. Serum concentrations of the vitamin D metabolites, 25-hydroxyvitamin D, and 1, 25-dihydroxvitamin D should be measured if there is no obvious malignancy and neither PTH nor PTHrP levels are elevated. An elevated serum concentration of calcidiol is indicative of vitamin D intoxication. However, an increased level of calcitriol may be due to direct intake, extrarenal production in granulomatous disease or lymphoma, or increased renal production.
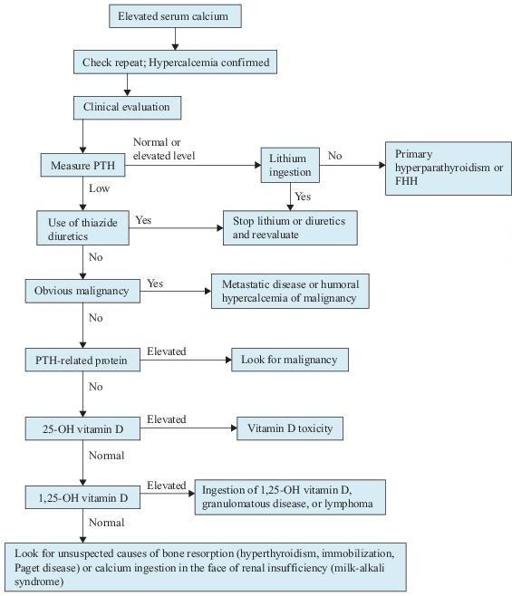
Figure 6–14
Algorithm for the workup of hypercalcemia. FHH, familial hypocalciuric hypercalcemia; PTH, parathyroid hormone.
TABLE 6–8. Laboratory Results in Common Causes of Hypercalcemia
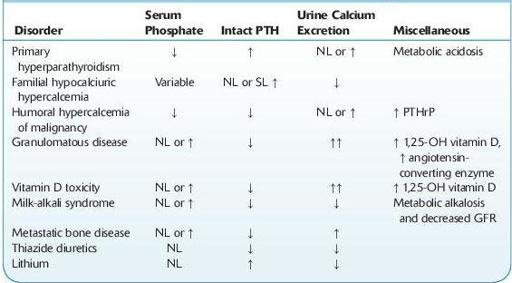
NL, normal level; PTHrP, parathyroid hormone–related protein; SL, slightly.
Normal values: urine calcium: 100–250 mg/24 h (females) and 100–300 mg/24 h (males); serum phosphate: 2.5–4.5 mg/dL; PTH (intact): 12–72 pg/mL; 1,25-OH Vitamin D: 14–78 pg/mL; angiotensin-converting enzyme: 17–70 units; PTHrP: <2.8 pmol/L.
Suggested Readings
Agus ZS. Clinical manifestations of hypercalcemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Agus ZS. Diagnostic approach to hypercalcemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Agus ZS. Etiology of hypercalcemia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
OSTEOPOROSIS
Definition
The World Health Organization defines osteoporosis as bone mineral density (BMD) more than 2.5 standard deviations below the mean of young normal controls (T-score).
Overview