Fundamentals of Midwifery: A Textbook for Students (62 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
5.12Mb size Format: txt, pdf, ePub
British Medical Journal
343, p. d7400 doi: 10. 1136/bmj.d7400Care Quality Commission (2014)
About us
. [Online], Available: http://www.cqc.org.uk/about-us [13 Mar 2014].Davis-Floyd, R. (2001) The technocractic, humanistic and holistic paradigms of childbirth.
International Journal of Gynaecology and Obstetrics
75, pp. S5–S23.Department of Health (2010)
Equity and excellence: Liberating the NHS
. Gateway reference 14385. London: Crown.Department of Health (2008)
High Quality Care for All: NHS Next Stage Review Final Report (Darzi)
. London: Department of Health.Department of Health (2007)
Maternity Matters: Choice, accessandcontinuity of care in asafe service
. London: HMSO.Department of Health (2004)
National Health Service Framework for children, young people and maternity services: Maternity Services
. London: HMSO.Department of Health (1993)
Changing Childbirth Part 1: Report of the Expert Maternity Group
. London: HMSO.Department of Health, Public Health England (2013)
Midwifery Services for improves health and well-being
[Available online] www.gov.uk/government/publications/midwifery-services-for-improved-health-and-wellbeingDevane, D., Brennan, M., Begley, C., et al. (2010) A systematic review, meta-analysis, meta-synthesis, and economic analysis of midwife-led models of care. Royal College of Midwives: London.
 140Edwards, N. (2005)
140Edwards, N. (2005)
Birthing Autonomy Women’s Experiences of Planning Home Births
, 1st edn. Oxon: Routledge.Freeman, L.M., Adair, V., Timperley, H., West, S.H. (2006) The influence of birthplace and models of care on midwifery practice for the management of women in labour.
Women and Birth
19, pp. 97–105.Gagnon, A.J., Sandall, J. (2011) Individual or group antenatal education for childbirth or parenthood, or both (Review).
The Cochrane Collaboration
Issue 10 Available at http://www.thecochranelibrary.com Wiley Ltd.Green, J., Baston, H., Easton, S., McCormick, F. (2003)
Greater Expectations?
Summary report. Mother infant Research Unit (MIRU), University of Leeds.Harrison, M.J., Kushner, K.E., Benzies, K., Rempel, G.K. (2003) Women’s satisfaction with their involvement in health care decisions during a high-risk pregnancy.
Birth
30 (2 June), pp. 109–115.Healthwatch (2014)
About us
. [Online], Available: http://www.healthwatch.co.uk/about-us [16 Mar 2014].Hunter, B., Berg, M., Lundgren, I., Olafsdottir, O.A., Kirkham, M. (2008) Relationships: The hidden threads in a tapestry of maternity care.
Midwifery
24 (2), pp. 132–137.Johanson, R., Newburn, M., MacFarlane, A. (2002) Has the medicalisation of childbirth gone too far?
British Medical Journal
324, pp. 892–895.Jomeen, J., Martin, C.R. (2005) Self-esteem and mental health during early pregnancy.
Clinical Effectiveness in Nursing
Mar–June 9 (1–2), pp. 92–95.Jomeen, J. (2010)
Choice, control and contemporary childbirth understanding through women’s stories
, 1st edn. United Kingdom: Radcliffe Publishing.Kirkham, M. (ed.) (2010)
The Midwife-Mother Relationship
, 2nd edn. England: Palgrave Macmillan.Lab tests online UK (2013)
Full Blood Count
. [Online]. Available: http://www.labtestsonline.org.uk/ understanding/analytes/fbc/tab/testLambert, C. (2013)
The influence of self in women’s decision-making about birthplace: An Interpretive Phenom- enological Study
. Doctoral Thesis University of Hull. Hull.Levy, V. (1999) Protective Steering: A grounded theory study of the processes by which midwives facilitate informed choices during pregnancy.
Journal of Advanced Nursing
29 (1), pp. 104–112.Marinac-Dabic, D., Krulewitch, C.J., Moore, R.M. Jr. (2002) The safety of prenatal ultrasound exposure in human studies.
Epidemiology
13 (3), pp. 19–S22.Marshall, J., Raynor, M. (2014)
Myles Textbook for Midwives
, 16th edn. Edinburgh: Elsevier. Martin, E.A. (2010)
Concise Oxford Colour Medical Dictionary
. Oxford: Oxford University Press.McMillan, A., Barlow, J., Redshaw, M. (2009) Preparation for birth and beyond. A resource pack for leaders of community groups and activities. Available at: http://www.yor-ok.org.uk/Downloads/Parenting/ Preparation%20for%20Birth%20and%20Beyond.pdfMoffat, M.A., Bell, J.S., Porter, M.A., Lawton, S., Hundley, V., Danielian, S., Bhattacharya, S. (2007) Decision making about mode of delivery among pregnant women who have previously had a caesarean section: a qualitative study.
MIDIRS Midwifery Digest
17 (2), pp. 210–221.National Institute for Clinical Excellence (2007)
Antenatal and Postnatal Mental Health; Clinical Management and Service Guidance
. London: Department of Health.National Institute for Health and Clinical Excellence (2008)
Routine antenatal anti-D prophylaxis for women who are rhesus D negative Review of NICE technology appraisal guidance 41
. London: NICE.National Institute for Health and Clinical Excellence (2008)
Antenatal Care: Routine care for healthy pregnant women
. Full Guideline. London: NICE.National Institute for Health and Clinical Excellence (2010)
Antenatal Care: Routine care for the healthy pregnant woman NICE clinical guideline 62
. London: NICE.National Institute for Health and Clinical Excellence (2010)
Quick reference guide Hypertension in pregnancy guideline 107
. London: NICE.Neighbourhood Midwives (2013)
Our service
. [Online], Available: http://www.neighbourhoodmidwives
343, p. d7400 doi: 10. 1136/bmj.d7400Care Quality Commission (2014)
About us
. [Online], Available: http://www.cqc.org.uk/about-us [13 Mar 2014].Davis-Floyd, R. (2001) The technocractic, humanistic and holistic paradigms of childbirth.
International Journal of Gynaecology and Obstetrics
75, pp. S5–S23.Department of Health (2010)
Equity and excellence: Liberating the NHS
. Gateway reference 14385. London: Crown.Department of Health (2008)
High Quality Care for All: NHS Next Stage Review Final Report (Darzi)
. London: Department of Health.Department of Health (2007)
Maternity Matters: Choice, accessandcontinuity of care in asafe service
. London: HMSO.Department of Health (2004)
National Health Service Framework for children, young people and maternity services: Maternity Services
. London: HMSO.Department of Health (1993)
Changing Childbirth Part 1: Report of the Expert Maternity Group
. London: HMSO.Department of Health, Public Health England (2013)
Midwifery Services for improves health and well-being
[Available online] www.gov.uk/government/publications/midwifery-services-for-improved-health-and-wellbeingDevane, D., Brennan, M., Begley, C., et al. (2010) A systematic review, meta-analysis, meta-synthesis, and economic analysis of midwife-led models of care. Royal College of Midwives: London.
 140Edwards, N. (2005)
140Edwards, N. (2005)Birthing Autonomy Women’s Experiences of Planning Home Births
, 1st edn. Oxon: Routledge.Freeman, L.M., Adair, V., Timperley, H., West, S.H. (2006) The influence of birthplace and models of care on midwifery practice for the management of women in labour.
Women and Birth
19, pp. 97–105.Gagnon, A.J., Sandall, J. (2011) Individual or group antenatal education for childbirth or parenthood, or both (Review).
The Cochrane Collaboration
Issue 10 Available at http://www.thecochranelibrary.com Wiley Ltd.Green, J., Baston, H., Easton, S., McCormick, F. (2003)
Greater Expectations?
Summary report. Mother infant Research Unit (MIRU), University of Leeds.Harrison, M.J., Kushner, K.E., Benzies, K., Rempel, G.K. (2003) Women’s satisfaction with their involvement in health care decisions during a high-risk pregnancy.
Birth
30 (2 June), pp. 109–115.Healthwatch (2014)
About us
. [Online], Available: http://www.healthwatch.co.uk/about-us [16 Mar 2014].Hunter, B., Berg, M., Lundgren, I., Olafsdottir, O.A., Kirkham, M. (2008) Relationships: The hidden threads in a tapestry of maternity care.
Midwifery
24 (2), pp. 132–137.Johanson, R., Newburn, M., MacFarlane, A. (2002) Has the medicalisation of childbirth gone too far?
British Medical Journal
324, pp. 892–895.Jomeen, J., Martin, C.R. (2005) Self-esteem and mental health during early pregnancy.
Clinical Effectiveness in Nursing
Mar–June 9 (1–2), pp. 92–95.Jomeen, J. (2010)
Choice, control and contemporary childbirth understanding through women’s stories
, 1st edn. United Kingdom: Radcliffe Publishing.Kirkham, M. (ed.) (2010)
The Midwife-Mother Relationship
, 2nd edn. England: Palgrave Macmillan.Lab tests online UK (2013)
Full Blood Count
. [Online]. Available: http://www.labtestsonline.org.uk/ understanding/analytes/fbc/tab/testLambert, C. (2013)
The influence of self in women’s decision-making about birthplace: An Interpretive Phenom- enological Study
. Doctoral Thesis University of Hull. Hull.Levy, V. (1999) Protective Steering: A grounded theory study of the processes by which midwives facilitate informed choices during pregnancy.
Journal of Advanced Nursing
29 (1), pp. 104–112.Marinac-Dabic, D., Krulewitch, C.J., Moore, R.M. Jr. (2002) The safety of prenatal ultrasound exposure in human studies.
Epidemiology
13 (3), pp. 19–S22.Marshall, J., Raynor, M. (2014)
Myles Textbook for Midwives
, 16th edn. Edinburgh: Elsevier. Martin, E.A. (2010)
Concise Oxford Colour Medical Dictionary
. Oxford: Oxford University Press.McMillan, A., Barlow, J., Redshaw, M. (2009) Preparation for birth and beyond. A resource pack for leaders of community groups and activities. Available at: http://www.yor-ok.org.uk/Downloads/Parenting/ Preparation%20for%20Birth%20and%20Beyond.pdfMoffat, M.A., Bell, J.S., Porter, M.A., Lawton, S., Hundley, V., Danielian, S., Bhattacharya, S. (2007) Decision making about mode of delivery among pregnant women who have previously had a caesarean section: a qualitative study.
MIDIRS Midwifery Digest
17 (2), pp. 210–221.National Institute for Clinical Excellence (2007)
Antenatal and Postnatal Mental Health; Clinical Management and Service Guidance
. London: Department of Health.National Institute for Health and Clinical Excellence (2008)
Routine antenatal anti-D prophylaxis for women who are rhesus D negative Review of NICE technology appraisal guidance 41
. London: NICE.National Institute for Health and Clinical Excellence (2008)
Antenatal Care: Routine care for healthy pregnant women
. Full Guideline. London: NICE.National Institute for Health and Clinical Excellence (2010)
Antenatal Care: Routine care for the healthy pregnant woman NICE clinical guideline 62
. London: NICE.National Institute for Health and Clinical Excellence (2010)
Quick reference guide Hypertension in pregnancy guideline 107
. London: NICE.Neighbourhood Midwives (2013)
Our service
. [Online], Available: http://www.neighbourhoodmidwives
rg.uk/midwifey-service.php [15 Mar 2014].Nolan, M.L. (2009) Information Giving and Education in Pregnancy: A Review of Qualitative Studies.
Journal of Perinatal Education
18 (4), pp. 21–30.Nursing & Midwifery Council (2012)
Midwives rules and standards
. London Publications: NMC.One to One (no date)
Our service
. [Online], Available: http://www.onetoonemidwives.org/our-service [15 June 2014].Powell Kennedy, H., Nardini, K., Mc-Leod-Waldo, R., Ennis, L. (2009) Top-selling childbirth advice books: a discourse analysis.
Birth
36 (4), pp. 318–324.Royal College of Obstetrics and Gynaecologists (RCOG) (2013)
Green Top Guideline 31: The investigation and management of small for gestational age fetus
. London: Royal College of Obstetrics and Gynaecologists.Sandall, J., Soltani, H., Gates Shennan, A., Devan, D. (2013) Midwife-led continuity models versus other models of care for childbearing women [Available on line] http://onlinelibrary.wiley.com/ cochranelibrary/Santalahti, P., Hemminki, E., Latikka, A., Ryynänen, M. (1998) Women’s decision-making in prenatal screen- ing.
Social Science & Medicine
46 (8), pp. 1067–1076.Stacey, C. (2011) Psychoneuroimmunology and wellbeing. In: Knight, A., McNaught, A.
Understanding Wellbeing: An Introduction for Students and Practitioners of Health and Social Care
. Banbury: Lantern.The King’s Fund (2014)
About us
. [Online], Available: http://www.kingsfund.org.uk/about-us [15 Mar 2014]. Tinkler, A., Quinney, D. (1998) Team Midwifery: the influence of the midwife-women relationship on women’s experiences and perceptions of maternity care.
Journal of Advanced Nursing
28 (1), pp.30–35.UK National Screening Committee (2014)
Screening Tests for You and Your Baby
. [Online], Available: http://www.screening.nhs.uk/getdata.php?id=17806UK National Screening Committee (2014) [online] Available: http://www.screening.nhs.uk/uknsc. Van de Vusse, L. (1999) Decision making in analyses of women’s birth stories.
Birth
26 (1), pp. 43–50.Wagner, M. (1994)
Pursuing the Birth Machine; The Search for Appropriate Birth Technology
. Australia: Ace Graphics.Walsh, D. (2012)
Evidence-based Care for normal Labour and Birth; A Guide for Midwives
, 2nd edn. London: Routledge.World Health Organization (WHO) (2012)
Guideline: Vitamin D supplementation in pregnant women
. Swit- zerland: World Health Organization. [Available online] http://www.who.int
 141
141
 Chapter 7
Chapter 7
Intrapartum midwifery careJulie Flint
University of Hull, Hull, UK
Sue Townend
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
 Learning outcomesBy the end of this chapter the reader will be able to:
Learning outcomesBy the end of this chapter the reader will be able to:
Journal of Perinatal Education
18 (4), pp. 21–30.Nursing & Midwifery Council (2012)
Midwives rules and standards
. London Publications: NMC.One to One (no date)
Our service
. [Online], Available: http://www.onetoonemidwives.org/our-service [15 June 2014].Powell Kennedy, H., Nardini, K., Mc-Leod-Waldo, R., Ennis, L. (2009) Top-selling childbirth advice books: a discourse analysis.
Birth
36 (4), pp. 318–324.Royal College of Obstetrics and Gynaecologists (RCOG) (2013)
Green Top Guideline 31: The investigation and management of small for gestational age fetus
. London: Royal College of Obstetrics and Gynaecologists.Sandall, J., Soltani, H., Gates Shennan, A., Devan, D. (2013) Midwife-led continuity models versus other models of care for childbearing women [Available on line] http://onlinelibrary.wiley.com/ cochranelibrary/Santalahti, P., Hemminki, E., Latikka, A., Ryynänen, M. (1998) Women’s decision-making in prenatal screen- ing.
Social Science & Medicine
46 (8), pp. 1067–1076.Stacey, C. (2011) Psychoneuroimmunology and wellbeing. In: Knight, A., McNaught, A.
Understanding Wellbeing: An Introduction for Students and Practitioners of Health and Social Care
. Banbury: Lantern.The King’s Fund (2014)
About us
. [Online], Available: http://www.kingsfund.org.uk/about-us [15 Mar 2014]. Tinkler, A., Quinney, D. (1998) Team Midwifery: the influence of the midwife-women relationship on women’s experiences and perceptions of maternity care.
Journal of Advanced Nursing
28 (1), pp.30–35.UK National Screening Committee (2014)
Screening Tests for You and Your Baby
. [Online], Available: http://www.screening.nhs.uk/getdata.php?id=17806UK National Screening Committee (2014) [online] Available: http://www.screening.nhs.uk/uknsc. Van de Vusse, L. (1999) Decision making in analyses of women’s birth stories.
Birth
26 (1), pp. 43–50.Wagner, M. (1994)
Pursuing the Birth Machine; The Search for Appropriate Birth Technology
. Australia: Ace Graphics.Walsh, D. (2012)
Evidence-based Care for normal Labour and Birth; A Guide for Midwives
, 2nd edn. London: Routledge.World Health Organization (WHO) (2012)
Guideline: Vitamin D supplementation in pregnant women
. Swit- zerland: World Health Organization. [Available online] http://www.who.int
 141
141 Chapter 7
Chapter 7Intrapartum midwifery careJulie Flint
University of Hull, Hull, UK
Sue Townend
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
 Learning outcomesBy the end of this chapter the reader will be able to:
Learning outcomesBy the end of this chapter the reader will be able to:explain parameters of normality in labour
discuss some of the challenges that midwives and women face in reducing the medicalisationof labour and birth
monitor the wellbeing of mothers and their unborn children in normal labour
determine when deviations from the norm may occur in the intrapartum period
provide evidence based care in the intrapartum setting.
Introduction
The emphasis of the midwife’s role in the provision of maternity care continues to lie within theboundaries of normal childbirth. The increasing rates of intervention in childbirth cause a great deal of debate, and the current medical model for childbirth is much criticised. It is paramount that student midwives base their knowledge and skills within the context of women centred care when pregnancy and birth are physiologically normal. Equally, as all women deserve the best care, all aspects of compassionate and competent care need to be applied to complex situ- ations to give all women and their babies the best start to family life.This chapter will focus on normal labour and birth and the role and responsibilities of the midwife, highlighting how an understanding of anatomy and physiology informs care provision and ensures a woman-centred approach. Place of birth and the influence of birth preparation education as a way to empower women are also included.
 Fundamentals of Midwifery: A Textbook for Students
Fundamentals of Midwifery: A Textbook for Students
, First Edition. Edited by Louise Lewis.© 2015 John Wiley & Sons, Ltd. Published 2015 by John Wiley & Sons, Ltd. Companion website: www.wileyfundamentalseries.com/midwifery
Facilitating and maintaining normality in childbirth
Thebirthofababyisatimewhenawomanhasanopportunitytodevelopasanindividualandreach her full potential; the support and care she receives can influence her outlook and progress throughout that journey and for the rest of her life. It is evident that if she feels some sense of per- sonal control of the situation, she may have a more positive experience and higher levels of satisfac- tion (Goodman et al. 2004). This can be achieved by having the ability to make choices about the place of birth that best suits her wherever possible; having some understanding of what is happen- ing to her through the process of labour and planning some coping strategies both prior to and during labour, making decisions along with the professionals giving care at the time (see Chapter 6:‘Antenatal midwifery care’where decision making is explored in greater depth).Those persons present at the time of labour and birth can influence the outcome both posi- tively and negatively, through their actions and words, with the potential to increase or decrease intervention. Often, this person is someone unknown to the woman. It is therefore essential for midwives to develop and feel confident in practising midwifery that is reflexive and adaptable within that midwife–woman relationship as explained by Kirkham (2010), in a gentle supportive manner. The midwifery role is one of expert practitioner. Practising as a skilled birth attendant (World Health Organization (WHO) 2004) requires an absolute grounding in the fundamental skills of midwifery which encompass the softer, caring and nurturing nature, sound knowledge base and clinical skills. This is what makes a midwife different and unique. A woman needs assurance that the person – the midwife she is putting her trust in – has the knowledge, skills and expertise including intuition, to care for her appropriately.It is during the intrapartum period that woman-centred care reaches the peak of importance for influencing the birthing experience. Women seek to have a carer who is ‘on their side’ one who discusses the benefits, risks and potential alternatives to any suggested interventions; allowing the women to make her own informed choice. This can help to support women to have personal control, rather than the carer assuming responsibility for knowing best and choosing options from a menu of actions to assist the woman (Kirkham 2004).The more straightforward and uncomplicated the birth, the greater the likelihood for the mother of achieving skin-to-skin contact with her baby, enjoying that first meeting and encour- aging the baby’s pre-feeding behaviours (Porter and Winberg 1999). The woman is less likely to have untoward outcomes such as genital tract trauma, suffer exhaustion or have undergone surgery. If the woman feels she has had a satisfactory experience she may feel increased self- worth, self-esteem and self-confidence in the transition into parenthood, with perhaps less potential for postnatal depression (Thompson et al. 2002).Armed with knowledge and compassion, the skill for the midwife is to provide safe, effective care for all women regardless of the level of complexity in the pregnancy or throughout the intrapartum period. Some women face challenges when they have hopes and choices that lie outside clinical guidance, or are hoping to prevent interventions they may feel are unnecessary when known medical conditions and situations become evident.Figure 7.1 Demonstrates how different pathways of care and intervention can lead to different outcomes in birth experience. The flow chart represents how the lead carer for the woman may fluctuate between the midwife and the obstetrician. Confusion may occur when the woman remains within the parameters of normality, monitored by midwives, but with varying degrees of intervention to achieve a vaginal birth, for example; pharmacological methods of pain relief, amniotomy, intravenous infusion and cardiotocograph (CTG) monitoring. The woman may
 143
143
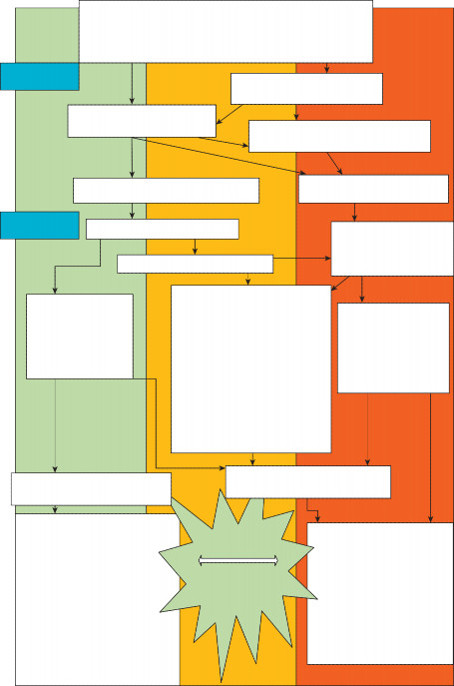 Direct access to Midwife or General Practitioner (GP) referral Midwife undertakes booking for care and screening Assesses any risks of ill health to mother and baby
Direct access to Midwife or General Practitioner (GP) referral Midwife undertakes booking for care and screening Assesses any risks of ill health to mother and baby
Pregnancy
Medical review of case by consultant obstetrician
 144
144
Midwifery monitored care throughout pregnancy
Referred or regular consultant review if high or developing risk of ill health
Onset of Labour at home or birth centre
Onset of labour in obstetric unit
Labour
Midwifery monitored care
Possible transfer to obstetric unit
Midwifery monitored care with medical availability/ input
Physiological normal birth
No intervention
Normal vaginal birth with varying degrees of intervention which may include;
Introduction
The emphasis of the midwife’s role in the provision of maternity care continues to lie within theboundaries of normal childbirth. The increasing rates of intervention in childbirth cause a great deal of debate, and the current medical model for childbirth is much criticised. It is paramount that student midwives base their knowledge and skills within the context of women centred care when pregnancy and birth are physiologically normal. Equally, as all women deserve the best care, all aspects of compassionate and competent care need to be applied to complex situ- ations to give all women and their babies the best start to family life.This chapter will focus on normal labour and birth and the role and responsibilities of the midwife, highlighting how an understanding of anatomy and physiology informs care provision and ensures a woman-centred approach. Place of birth and the influence of birth preparation education as a way to empower women are also included.
 Fundamentals of Midwifery: A Textbook for Students
Fundamentals of Midwifery: A Textbook for Students, First Edition. Edited by Louise Lewis.© 2015 John Wiley & Sons, Ltd. Published 2015 by John Wiley & Sons, Ltd. Companion website: www.wileyfundamentalseries.com/midwifery
Facilitating and maintaining normality in childbirth
Thebirthofababyisatimewhenawomanhasanopportunitytodevelopasanindividualandreach her full potential; the support and care she receives can influence her outlook and progress throughout that journey and for the rest of her life. It is evident that if she feels some sense of per- sonal control of the situation, she may have a more positive experience and higher levels of satisfac- tion (Goodman et al. 2004). This can be achieved by having the ability to make choices about the place of birth that best suits her wherever possible; having some understanding of what is happen- ing to her through the process of labour and planning some coping strategies both prior to and during labour, making decisions along with the professionals giving care at the time (see Chapter 6:‘Antenatal midwifery care’where decision making is explored in greater depth).Those persons present at the time of labour and birth can influence the outcome both posi- tively and negatively, through their actions and words, with the potential to increase or decrease intervention. Often, this person is someone unknown to the woman. It is therefore essential for midwives to develop and feel confident in practising midwifery that is reflexive and adaptable within that midwife–woman relationship as explained by Kirkham (2010), in a gentle supportive manner. The midwifery role is one of expert practitioner. Practising as a skilled birth attendant (World Health Organization (WHO) 2004) requires an absolute grounding in the fundamental skills of midwifery which encompass the softer, caring and nurturing nature, sound knowledge base and clinical skills. This is what makes a midwife different and unique. A woman needs assurance that the person – the midwife she is putting her trust in – has the knowledge, skills and expertise including intuition, to care for her appropriately.It is during the intrapartum period that woman-centred care reaches the peak of importance for influencing the birthing experience. Women seek to have a carer who is ‘on their side’ one who discusses the benefits, risks and potential alternatives to any suggested interventions; allowing the women to make her own informed choice. This can help to support women to have personal control, rather than the carer assuming responsibility for knowing best and choosing options from a menu of actions to assist the woman (Kirkham 2004).The more straightforward and uncomplicated the birth, the greater the likelihood for the mother of achieving skin-to-skin contact with her baby, enjoying that first meeting and encour- aging the baby’s pre-feeding behaviours (Porter and Winberg 1999). The woman is less likely to have untoward outcomes such as genital tract trauma, suffer exhaustion or have undergone surgery. If the woman feels she has had a satisfactory experience she may feel increased self- worth, self-esteem and self-confidence in the transition into parenthood, with perhaps less potential for postnatal depression (Thompson et al. 2002).Armed with knowledge and compassion, the skill for the midwife is to provide safe, effective care for all women regardless of the level of complexity in the pregnancy or throughout the intrapartum period. Some women face challenges when they have hopes and choices that lie outside clinical guidance, or are hoping to prevent interventions they may feel are unnecessary when known medical conditions and situations become evident.Figure 7.1 Demonstrates how different pathways of care and intervention can lead to different outcomes in birth experience. The flow chart represents how the lead carer for the woman may fluctuate between the midwife and the obstetrician. Confusion may occur when the woman remains within the parameters of normality, monitored by midwives, but with varying degrees of intervention to achieve a vaginal birth, for example; pharmacological methods of pain relief, amniotomy, intravenous infusion and cardiotocograph (CTG) monitoring. The woman may
 143
143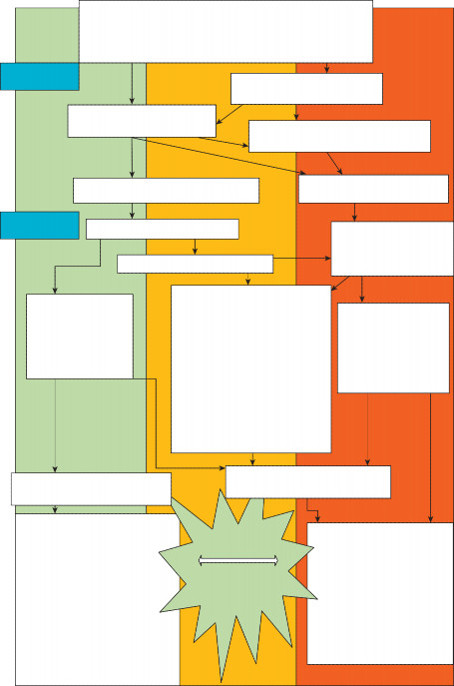 Direct access to Midwife or General Practitioner (GP) referral Midwife undertakes booking for care and screening Assesses any risks of ill health to mother and baby
Direct access to Midwife or General Practitioner (GP) referral Midwife undertakes booking for care and screening Assesses any risks of ill health to mother and babyPregnancy
Medical review of case by consultant obstetrician
 144
144Midwifery monitored care throughout pregnancy
Referred or regular consultant review if high or developing risk of ill health
Onset of Labour at home or birth centre
Onset of labour in obstetric unit
Labour
Midwifery monitored care
Possible transfer to obstetric unit
Midwifery monitored care with medical availability/ input
Physiological normal birth
No intervention
Normal vaginal birth with varying degrees of intervention which may include;
Other books
Encuentros (El lado B del amor) by Gabriel Rolón
Under the Canopy by Sorokin, Serg
Kiss Of Twilight by Loribelle Hunt
Broken Soup by Jenny Valentine
Mammoth Secrets by Ashley Elizabeth Ludwig
Machines of the Dead by David Bernstein
Switchers by Kate Thompson
Dying to Read by Lorena McCourtney
Just One Week by Alice Gaines
Betrayal Foretold: Descended of Dragons, Book 3 by Jen Crane