i bc27f85be50b71b1 (83 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

NE.RVOUS SYSTEM
277
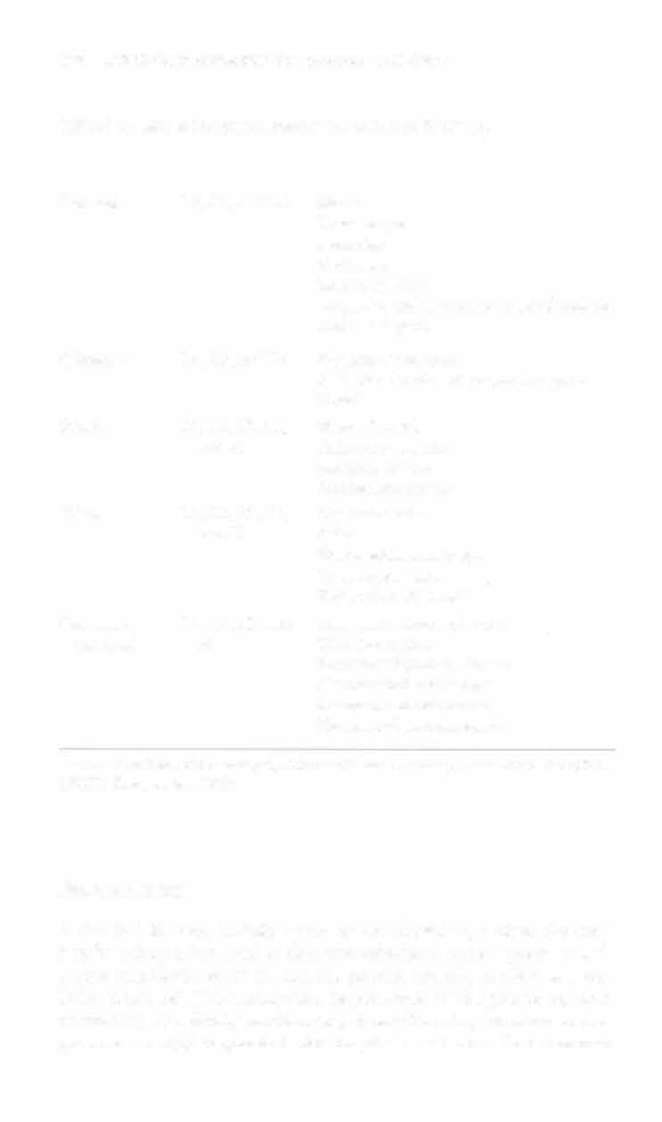
Table 4-7. Major Peripheral Nerves of the Upper Extremity
Nerve
Spinal RoO[
Innervation
Dorsal scapular
C5
Levaror scapulae, rhomboid major
and minor
Supmscapular
C5 and C6
Supraspinatus, infraspinatus
Lower
C5 and C6
Teres major
subscapular
Axillary
C5 and C6
Teres minor, delraid
Radial
C5, C6, C7,
Triceps, brachioradialis, anconeus,
and C8
extensor carpi radialis longus and
brevis, supinator, extensor carpi
ulnaris, extensor digirorum, extensor
digiti minimi, extensor indicis, extensor pollicis longus and brevis, abducror pollieis brevis
Ulnar
C8 and T I
Flexor digitorum profundus, flexor
carpi uln!lris, palmaris brevis, abducror digiti minimi, flexor digiti minimi
brevis, opponens digiti minimi, palmar and dorsal interossei, third and
fourth lumbricals
Median
C6, C7, C8,
Pronator teres, flexor carpi radialis, pal-
and T l
maris longus, flexor digirorum superficialis and profundus, flexor pallicis
longus, pronaror quadratus, abductor
pollicis brevis, opponens pollieis,
flexor pollicis brevis, first and second
lumbricals
Musculo
C5, C6, and C7
Coracobrachialis, brachialis, biceps
cutaneous
Source: Data from FH Nencr (cd). Arias of Human Anaromy. Summit Ciry, NJ: CIBA
GEIGY Corporation, 1989.
Neurologic Examination
The neurologic examination is initiated on hospital admission or in
the field and is reassessed continuously, hourly or daily, as necessary.
The neurologic examination consists of patient history; mental status
examination; viral sign measurement; vision, motor, sensory, and
coordination testing; and diagnostic resring.
278 AClITE CARE HANDBOOK FOR PHYSICAL Tt-IE.RAI)ISTS
Table 4-8. Major Peripheral Nerves of the Lower Extremiry
Nerve
Spinal Root
Innervation
Femoral
L2, U, and L4
Iliacus
Psoas major
Sartorius
Pecrinous
Rectus femoris
Vastus lateral is, intermedius, and medialis
Articularis genu
Obturator
L2, L3, and L4
Obturator extern LIS
Adductor brevis, longus, and magnus
Gracilis
Sciatic
L4, LS, 5 1 , S2,
Biceps femoris
and S3
Adductor magnus
Semitendinosus
Semimembranosus
Tibial
L4, LS, S], 52,
Gastrocnemius
and S3
Soleus
Flexor digitorum longus
Tibialis posterior
Flexor hallucis longus
Common
L4, LS, S l , and
Peroneus longus and brevis
peroneal
S2
Tibialis amerior
Extensor digitorum longus
Extensor hallucis longus
Extensor hallucis brevis
Extensor digitorum brevis
Source: Dara from FH Nener (cd). Arias of I-Iuman Anawmy. Summir Ciry, Nl: CI8A
GEIGY Corporarion, 1989.
Patietlt History
A detailed history, initially taken by the physician, is often the most
helpful information used to delineate whether a patient presents with
a true neurologic event or another process (usually cardiac or metabolic in nature). The history may be presented by the patient or, more commonly, by a family member or person witnessing the acme or progressive event(s) responsible for hospital admission. One common
NERVOUS SYSTEM
279
Table 4-9. Major Peripheral Nerves of the Trunk
Nerve
Spinal Root
Innervation
Spinal accessory
C3 and C4
Trapezius
Phrenic
C3, C4, and C5
Diaphragm
Long thoracic
C5, C6, and C7
Serratus anterior
Medial pecroral
C6, C7, and C8
Pectoralis minor and
major
Lateral pecroral
C7, C8, and T I
Pectoralis major
Thoracodorsal
C 7 and C8
Latissimus dorsi
Intercostal
Corresponds ro nerve
External intercostals
root level
Internal intercosrals
Levatores costarum longi
and brevis
Iliohypogastric and
L I
Transversus abdominus
ilioinguinal
Internal abdominal
oblique
Inferior gluteal
L4, L5, 51, and 52
Gluteus maximus
Superior gluteal
L4, L5, and 5'1
Gluteus medius and
minlmus
Tensor fascia lame
Source: Data from FH Netter (cd). Arias of Human Anatomy. Summit City, NJ: eIBA
GEIGY Corporation, 1989.
framework for organizing questions regarding each neurologic complaint, sign, or symprom is presented here7,8:
• What is the patient feeling?
•
When did the problem initially occur and has it progressed?
•
What relieves or exacerbates the problem?
• What is the onset, frequency, and duration of signs or symptoms?
In addition to the general medical record review (see Appendix 1-
A), questions relevant to a complete neurologic history include the
following:
• Does the problem involve loss of consciousness?
•
Did a fall precede or follow the problem?

280
AClfrE CARE HANDBOOK FOR PHYSICAl H1FRAPISTS
Vlnuall)tlal
UM of upper
limb
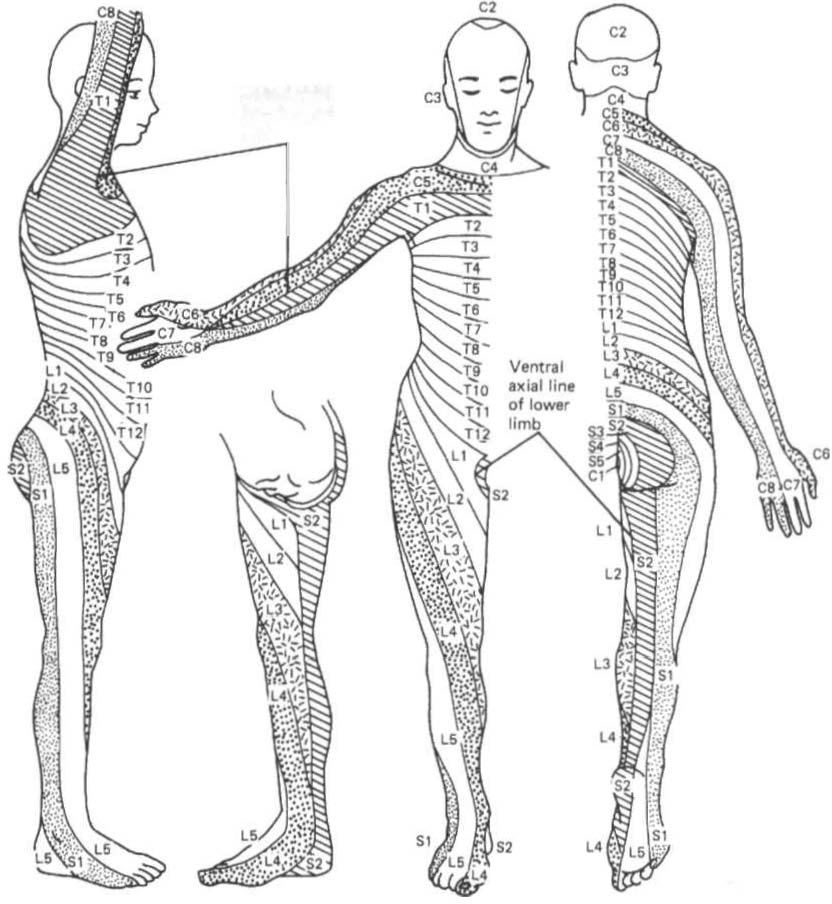
Figure 4-6. Dermatome chart based 0" embryologic segments. (\vith permission from CD Maitland /ed/. Vertebral Manipulation /5th edt. Oxford, UK: Butterworth-H einemallll, 1986;46.)
•
Is there headache, dizziness, or visual disturbance?
•
What are the functional deficits associated with the problem?
•
Is there an alteration of speech?
•
Does the patient demonstrate memory loss or altered cognition?