Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics
Pediatric Primary Care Case Studies (100 page)

• Poor capability of the parents to monitor and care for their child
• Winter season
If the child in question has one or more of these risk factors, there is concern for dehydration, especially during the first 6 hours of a primary infection such as rotavirus. For a telephone assessment, the provider’s knowledge of the patient’s family is crucial in assessing the validity of the information.
In addition to family data, the following information related to the specific illness is essential in assessing the child’s condition and determining if he or she should be seen in the office:
• Age of child
• Onset and duration of the illness
• Number of diarrhea and vomiting episodes
• Presence of blood or mucus in the stool
• Intake of fluids—what and how much over the past 24 hours
• Moisture on the mucus membranes
• Fever
• Urine frequency, amount, color, and last void
• Activity of the child
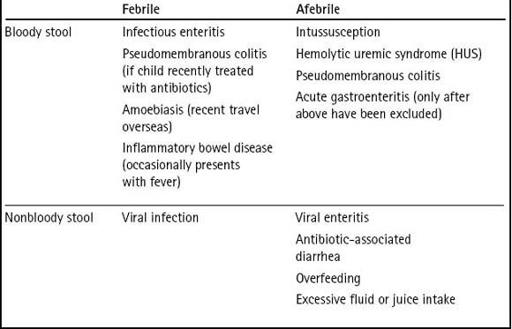
Assessing fever and bloody stool, two features that can be present in gastroenteritis, is particularly helpful in determining the differential diagnosis and guiding the provider to make appropriate decisions regarding care (see
Table 25-1
).
The above information, along with the season of the year, can help guide the provider in diagnosing and treating the child. However, in order to distinguish an acute self-limited episode of gastroenteritis from a more serious disorder, additional historical information must be obtained, including:
• Contacts with ill individuals
• Exposures to illness or environmental contaminants such as in daycare, travel, water source, or foods
• Previous episodes of gastroenteritis or dehydration (how many and time of last episode)
• Medications being taken, including over-the-counter or prescription, and any complementary or alternative medications or herbal remedies
• Prior history of other significant infections
Table 25–1 Differential Diagnosis of Gastroenteritis by Fever and Bloody Stool
• Presence of concurrent infections
• Underlying diseases
• History of allergies
• Family history of gastrointestinal conditions
For the child who is seen in person, the provider needs to assess and evaluate the following:
• The infant’s or child’s level of consciousness; activity and energy level
• Vital signs
• Signs of dehydration
• A careful abdominal exam looking for the presence of any localizing and/or meningeal signs
What additional questions will you need to ask when you return Sara’s mother’s phone call?
With the information from the office triage nurse and a review of Sara’s records that indicate she is up-to-date on her immunizations, has no known allergies to medications or food, no family history of gastrointestinal conditions, and no history of recent hospitalization or serious illness, you telephone Sara’s mother. You ask her the following questions:

How long has Sara been sick? What started first, the vomiting or the diarrhea?
She had been fine until just a few days ago. Two days ago, she threw up twice and then she had the loose stools. She had four loose stools today.

What do the stools look like? Any blood or mucus?
They are loose greenish stools. There doesn’t seem to be any blood in them.

When did her fever start, what has it been, and how have you dealt with her fever?
I first noticed she felt hot last night about 9 p.m. Her temperature was 100°F. I gave her some Tylenol, and it came down to normal within an hour. Her temperature this morning was 99.8°F. I haven’t given her anything for fever today, and she really doesn’t feel very warm now.

Is anybody in the family sick? Have you traveled anywhere recently? Has Sara eaten any new foods? Is Sara in daycare?
Nobody in the family is ill. We have not gone anywhere lately. Sara’s been eating her normal diet, but we did change daycare about 2 weeks ago to a center nearer to home.

Has Sara been eating and drinking? How many times has Sara voided today including the time of her last urination
? She had some dry cereal and milk today and some peaches for lunch, and she didn’t vomit after eating this time. She has gone to the bathroom at least three times to void, with her last voiding about 2 hours ago.

Has she been playing or lying around napping?
She has been playing with her dolls this morning and watched one of her videos this afternoon. Do you think something else is wrong with her since she has been sick so much this year? What am I doing wrong?
You reassure Sara’s mom that she isn’t doing anything wrong, though you understand how anxious she is because Sara is sick again.
What are the possible differential diagnoses?

