Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (21 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
6.34Mb size Format: txt, pdf, ePub
• All beats look similar; predominantly upward in V
1
= RBBB-type vs. downward = LBBB-type
• In structurally
abnormal
heart:
prior MI
(scar);
CMP
;
myocarditis
;
arrhythmogenic RV CMP (ARVC)
: incomplete RBBB,
ε wave (terminal notch in QRS) & TWI in V
1
–V
3
on resting ECG, LBBB-type VT, dx w/ MRI (
Lancet
2009;373:1289)
• In structurally
normal
heart (w/ normal resting ECG):
RVOT VT
: LBBB-type VT w/ inferior axis; typically ablate
idiopathic LV VT
: RBBB-type VT w/ superior axis; responds to verapamil
Polymorphic ventricular tachycardia (PMVT)
• QRS morphology changes from beat to beat • Etiologies:
ischemia
;
CMP
; catecholaminergic;
torsades de pointes
(TdP = “twisting of the points,” PMVT + ↑ QT): ↑ QT
acquired
(meds, lytes, stroke, see "ECG") w/ risk ↑ w/ ↓ HR, freq PVCs (pause dependent)
or
congenital
(K/Na channelopathies) w/ resting Tw abnl & TdP triggered by sympathetic stimulation (eg, exercise, emotion, sudden loud noises) (
Lancet
2008;372:750).
Brugada syndrome
(Na channelopathy):>
; pseudo-RBBB w/ STE in V
1
–V
3
(provoked w/ class IA or IC) on resting ECG
Diagnostic clues that favor VT (assume until proven o/w)
•
Prior MI
,
CHF
or
LV dysfunction
best predictors
that WCT is VT (
Am J Med
1998;84:53) • Hemodynamics and rate do
not
reliably distinguish VT from SVT
• MMVT is regular, but initially it may be slightly irregular, mimicking AF w/ aberrancy;
grossly
irregularly irregular rhythm suggests AF w/ aberrancy • ECG features that favor VT (
Circ
1991;83:1649)
AV dissociation
(independent P waves, capture or fusion beats) proves VT
very wide QRS
(>140 ms in RBBB-type or >160 in LBBB-type);
extreme axis deviation
QRS morphology atypical for BBB
RBBB-type: absence of tall R′ (or presence of monophasic R) in V
1
, r/S ratio <1 in V
6
LBBB-type: onset to nadir >60–100 ms in V
1
, q wave in V
6
concordance
(QRS in all precordial leads w/ same pattern/direction)
Long-term management (
JACC
2006;48:1064)
• Workup:
echo
to ✓ LV fxn,
cath
or
stress test
to r/o ischemia, ? MRI and/or RV bx to
look for infiltrative CMP or ARVC, ?
EP study
to assess inducibility
•
ICD
: 2° prevention after documented VT/VF arrest (unless due to reversible cause)
1° prev. if high risk, eg, EF <30–35%, ARVC, Brugada, certain LQTS, severe HCMP. See “Intracardiac Devices.” ? Wearable vest if revers. etiol. waiting for ICD (
Circ
2013;127:854).
Antitachycardia pacing (ATP = burst pacing faster than VT) can terminate VT w/o shock
•
Meds
: bB, antiarrhythmics (eg, amio, mexiletine) to suppress VT which could trigger shock • If med a/w TdP → QT >500 ± VPBs: d/c med, replete K, give Mg, ± pacing (
JACC
2010;55:934) •
Radiofrequency ablation
if isolated VT focus or if recurrent VT triggering ICD firing; ablation before ICD implantation ↓ discharge rate by 40% (
Lancet
2010;375:31)
ATRIAL FIBRILLATION
Classification (
Circ
2006;114:e257 & 2011;123:104)
•
Paroxysmal
(self-terminating, usually <48 h) vs.
persistent
(sustained >7 d or terminated after Rx) vs.
permanent
(typically >1 y and when cardioversion has failed or is foregone) •
Valvular
(rheumatic MV disease, prosthetic valve or valve repair) vs.
nonvalvular
•
Lone AF
= age <60 y and w/o clinical or echo evidence of cardiac disease (including HTN)
Epidemiology and etiologies (
Annals
2008;149:ITC5-2)
• 1–2% of pop. has AF (8% of elderly); lifetime risk 25%; mean age at presentation ~75 y • Acute (up to 50% w/o identifiable cause)
Cardiac
: HF, myo/pericarditis, ischemia/MI, hypertensive crisis, cardiac surgery
Pulmonary
: acute pulmonary disease or hypoxia (eg, COPD flare, PNA), PE, OSA
Metabolic
: high catecholamine states (stress, infection, postop, pheo), thyrotoxicosis
Drugs
: alcohol (“holiday heart”), cocaine, amphetamines, theophylline, caffeine
Neurogenic
: subarachnoid hemorrhage, ischemic stroke
• Chronic: ↑ age, HTN, ischemia, valve dis. (MV, TV, AoV), CMP, hyperthyroidism, obesity
Evaluation
• H&P, ECG, CXR, TTE (LA size, thrombus, valves, LV fxn, pericardium), K, Mg, FOBT before anticoag, TFTs; r/o MI not necessary unless other ischemic sx
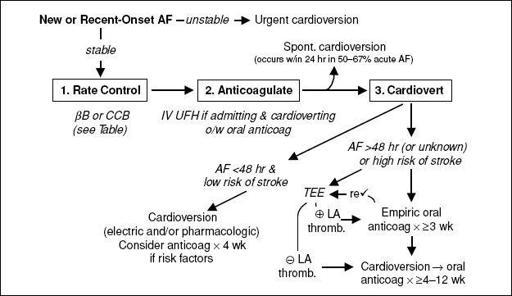
Figure 1-5
Approach to acute AF
(Adapted from
NEJM
2004;351:2408;
JACC
2006;48:e149)
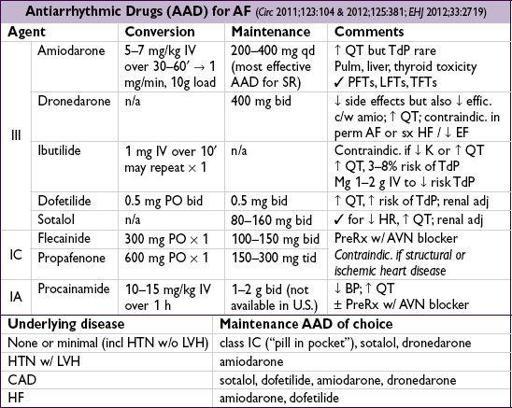
Strategies for recurrent AF (
Circ
2011;123:104;
Lancet
2012;379:648)
•
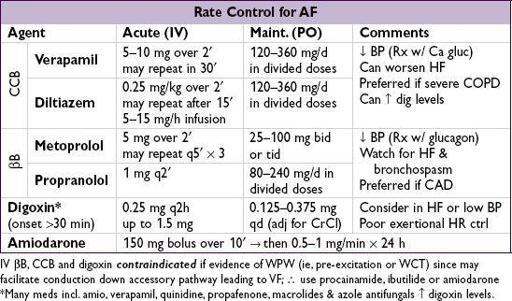
Rate control
: goal HR <110 at rest if EF >40% and asx (
NEJM
2010;362:1363)
AV node ablation + PPM as a last resort (
NEJM
2001;344:1043; 2002;346:2062)
•
Rhythm control
: no clear survival benefit vs. rate cntl (
NEJM
2002;347:1825 & 2008;358:2667)
Consider if
sx
w/ rate cntl, difficult to cntl rate, ? unable to anticoag, ? benefit in CRT
Other books
Mona Lisa Overdrive by William Gibson
Children of Fire by Drew Karpyshyn
One E-mail: (BBW Romance) (One Soldier Series) by Lovell, Christin
Incriminated by M. G. Reyes
Maximum Risk by Lowery, Jennifer
We Are All Completely Beside Ourselves by Karen Joy Fowler
Tara The Great [Nuworld 2] by Lorie O'Claire
The King's Key by Cameron Stelzer
Tote Bags and Toe Tags by Dorothy Howell