Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (18 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
8.52Mb size Format: txt, pdf, ePub
diet: rich in fruits & vegetables, low in saturated & total fat (DASH,
NEJM
2001;344:3)
sodium restriction: ≤2.4 g/d and ideally ≤1.5 g/d (
NEJM
2010;362:2102)
limit alcohol consumption: ≤2 drinks/d in men; ≤1 drink/d in women & lighter-wt Pts
•
Pharmacologic options
(if HTN
or
pre-HTN + diabetes or renal disease)
Pre-HTN
: ARB prevents onset of HTN, no ↓ in clinical events (
NEJM
2006;354:1685)
HTN
:
choice of therapy controversial, concomitant disease and stage may help guide Rx
uncomplicated
: thiazide if likely salt sensitive (eg, elderly, black, obese), o/w start w/ ACEI or CCB (
NEJM
2009;361:2153). bB not first line (
Lancet
2005;366:1545).
+
high-risk CAD
: ACEI or ARB (
NEJM
2008;358:1547); ACEI + CCB superior to ACEI + thiazide (
NEJM
2008;359:2417) or bB + diuretic (
Lancet
2005;366:895)
+
angina
: bB, CCB, nitrates
+
post-MI
: ACEI, bB ± aldosterone antagonist (see “ACS”)
+
HF
: ACEI/ARB, bB, diuretics, aldosterone antagonist (see “Heart Failure”)
+
2
°
stroke prevention
: ACEI (
Lancet
2001;358:1033); ? ARB (
NEJM
2008;359:1225) +
diabetes mellitus
: ACEI or ARB; can also consider diuretic, bB or CCB
+
chronic kidney disease
: ACEI/ARB (
NEJM
1993;329:1456 & 2001;345:851 & 861)
•
Tailoring therapy
if stage 1, start w/ monoRx; if not at goal, Δ to different class rather than adding 2nd agent
if stage 2, consider starting w/ combo (eg, ACEI + CCB;
NEJM
2008;359:2417) as most will require ≥2 drugs; low–mod doses of 2 drugs generally preferred over max dose of 1 drug (b/c of dose-related AEs)
if resistant [= HTN despite ≥3 drugs (incl diuretic) at opt doses], consider noncompliance, volume overload, secondary causes; ? renal artery denervation (
Lancet
2010;376:1903)
•
Secondary causes
Renovascular
: control BP w/ diuretic + ACEI/ARB (watch for ↑ Cr w/ bilat. RAS) or CCB Atherosclerosis risk-factor modification: quit smoking, ↓ chol. If refractory HTN, recurrent flash pulm edema, worse CKD, consider revasc
For atherosclerosis: stenting ↓ restenosis vs. PTA alone, but no clear improvement in BP or renal function vs. med Rx (
NEJM
2009;361:1953;
Annals
2009;150:840)
For FMD (usually more distal lesions): PTA ± bailout stenting
Renal parenchymal disease
: salt and fluid restriction, ± diuretics
Endocrine etiologies
: see “Adrenal Disorders”
•
Pregnancy:
methyldopa, labetalol, nifedipine, hydralazine; avoid diuretics; ACEI/ARB
HYPERTENSIVE CRISES
•
Hypertensive emergency
: ↑ BP → acute target-organ ischemia and damage
neurologic damage: encephalopathy, hemorrhagic or ischemic stroke, papilledema
cardiac damage: ACS, HF/pulmonary edema, aortic dissection
renal damage: proteinuria, hematuria, acute renal failure; scleroderma renal crisis
microangiopathic hemolytic anemia; preeclampsia-eclampsia
•
Hypertensive urgency
: SBP >180 or DBP >120 (?110) w/ min. or no target-organ damage
Precipitants
• Progression of essential HTN ± medical noncompliance (esp. clonidine) or Δ in diet • Progression of renovascular disease; acute glomerulonephritis; scleroderma; preeclampsia • Endocrine: pheochromocytoma, Cushing’s
• Sympathomimetics: cocaine, amphetamines, MAO inhibitors + foods rich in tyramine • Cerebral injury (do
not
treat HTN in acute ischemic stroke unless Pt getting lysed, extreme
BP (>220/120), Ao dissection, active ischemia or HF (
Stroke
2003;34:1056)
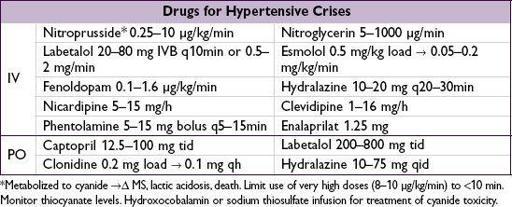
Treatment (
Chest
2007;131:1949)
• Tailor goals to clinical context (eg, more rapid lowering for Ao dissection) • Emergency: ↓ MAP by ~25% in
mins to 2 h
w/ IV agents (may need arterial line for monitoring); goal DBP <110 w/in 2–6 h, as tolerated • Urgency: ↓ BP in
hours
using PO agents; goal normal BP in ~1–2 d • Watch UOP, Cr, mental status: may indicate a lower BP is not tolerated
AORTIC ANEURYSMS
Definitions
•
True
aneurysm (dilation of all 3 layers of aorta) vs.
false
(rupture contained by adventitia) •
Location
: root (annuloaortic ectasia), thoracic aortic aneurysm (TAA), thoracoabdominal aortic aneurysm (TAAA), abdominal aortic aneurysm (AAA) •
Type
: fusiform (circumferential dilation) vs. saccular (localized dilation of aortic wall)
Epidemiology (
Circ
2010;121:e266;
Nat Rev Cardiol
2011;8:92)
• In U.S.,
15,000 deaths/y from aortic ruptures; overall
50,000 deaths/y from Ao disease •
TAA
::
1.7:1;
60% root/ascending Ao; 40% descending Ao; arch & TAAA rarer
Risk factors:
HTN
;
atherosclerosis
; congenital (
bicuspid AoV
, Turner’s);
connective tissue diseases
(Marfan, Ehlers-Danlos type IV, Loeys-Dietz);
aortitis
(Takayasu’s, GCA, spondyloarthritis, IgG4, syphilis); familial syndromes; chronic AoD; trauma
•
AAA
: ~4–8% prev. in those >65 y; 5–10× more common invs.
; mostly infrarenal
Risk factors = similar to
atherosclerosis
:
smoking
, HTN, hyperlipidemia, age, FHx
Pathophysiology (
NEJM
2009;361:1114;
Nat Med
2009;15:649)
•
LaPlace’s law
: tension across a cylinder ∝ [(ΔP × r) / (wall thickness)]
•
TAA
: medial degeneration = muscle apoptosis, elastin fiber weakening, mucoid infiltration •
AAA
: atherosclerosis & inflammation → matrix degeneration → medial weakening • Inflammatory and infectious (“mycotic”) aneurysms relatively rare
Screening (
Annals
2005;142:203;
JAMA
2009;302:2015;
Circ
2010;121:e266)
•
TAA
: no consensus guidelines; ? screen if bicuspid AoV or first-degree relative •
AAA
: ✓ for pulsatile abd mass; U/S>60 y w/ FHx of AAA &
65–75 y w/ prior tobacco
Diagnostic studies (
Circ
2005;111:816 & 2010;121:e266)
Other books
Lynna Banning by Wildwood
Teleny or the Reverse of the Medal by Oscar Wilde, Anonymous
The Presence by John Saul
The Mockingbird Next Door: Life With Harper Lee by Marja Mills
Forbidden Love: A BBW, BWWM Paranormal Romance by Mary T Williams
Silverbow by Simmons, Shannon
Rescuing Lilly by Miller, Hallie
Haunted Knights (Montbryce~The Next Generation Historical Romance) by Markland, Anna
Justice and Utu by David Hair
I Do! by Rachel Gibson