Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (16 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
3.4Mb size Format: txt, pdf, ePub
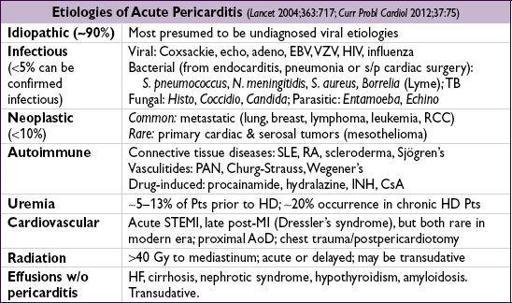
PERICARDIAL DISEASE
GENERAL PRINCIPLES
Anatomy
• 2-layered (parietal & visceral) tissue sac surrounding heart & proximal great vessels
Disease states
• Inflammation (w/ or w/o fluid accumulation) → pericarditis
• Fluid accumulation → effusion ± tamponade
• Decrease in compliance (sequela of inflammation) → constrictive pericarditis
• Tamponade and constriction characterized by increased ventricular interdependence
PERICARDITIS AND PERICARDIAL EFFUSION
Clinical manifestations (
NEJM
2004;351:2195)
•
Pericarditis
: retrosternal chest pain that is pleuritic, positional (↓ by sitting forward), radiates to trapezius; may be
absent
in tuberculous, neoplastic, post-XRT and uremic pericarditis; ± fever; ± s/s of systemic etiologies •
Effusion
: ranges from asx to tamponade (see below)
Physical exam
•
Pericarditis
: multiphasic
friction rub
best heard at LLSB w/ diaphragm of stethoscope. Notoriously variable and evanescent leathery sound w/ up to 3 components: atrial contraction, ventricular contraction, ventricular relaxation (
NEJM
2012;367:e20).
•
Effusion
: distant heart sounds, dullness over left posterior lung field due to compressive atelectasis from pericardial effusion (Ewart’s sign)
Diagnostic studies (
EHJ
2004;25:587;
Circ
2006;113:1622 & 2010;121:916)
• ECG: may show diffuse STE (
concave up
) & PR depression (except in aVR: ST ↓ & PR ↑), TWI; classically and in contrast to STEMI, TWI do not occur until STs normalize
Stages: (I) STE & PR ↓; (II) ST & PR normalize; (III) diffuse TWI; (IV) Tw normalize
ECG may show evidence of large effusion w/ low voltage & electrical alternans (beat-to- beat Δ in QRS amplitude and/or axis due to swinging heart)
• CXR: if large effusion (>250 mL of fluid) → ↑ cardiac silhouette w/ “water-bottle” heart and epicardial halo •
Echocardiogram
: presence, size, & location of
effusion
; presence of
tamponade physiology
; pericarditis itself w/o spec. abnl (∴ echo can be nl), although can see pericardial stranding (fibrin or tumor); can also detect LV/RV dysfxn (myocarditis ?) • CT will reveal pericardial effusions, often appearing larger than on echocardiography • CK-MB or troponin (in ~30%,
JACC
2003;42:2144) if myopericarditis. Consider CRP/ESR.
Workup for effusion
• r/o infxn: usually apparent from Hx & CXR; ? value of ✓ acute and convalescent serologies • r/o noninfectious etiologies: BUN, Cr, ANA, RF, HIV, screen for common malignancies • Pericardiocentesis if suspect infxn or malignancy or large effusion (>2 cm) or recurrent
✓ cell counts, TP, LDH, glc, Gram stain & Cx, AFB, cytology
ADA, PCR for MTb, and specific tumor markers as indicated by clinical suspicion
“exudate” criteria: TP >3 g/dL, TP
eff
/TP
serum
>0.5, LDH
eff
/LDH
serum
>0.6 or glc <60 mg/dL high Se (~90%) but
very low
Sp (~20%); overall low utility (
Chest
1997;111:1213)
• Pericardial bx if suspicion remains for malignancy or tuberculosis
Treatment of pericarditis (
EHJ
2004;25:587;
Circ
2006;113:1622)
• NSAIDs (eg, ibuprofen 600–800 mg tid × 7–14 d then taper) ± colchicine 1–2 mg × 1 → 0.5–1 mg bid × 3 mo (
Circ
2005;112:2012;
Heart
2012;98:1078); sx usually subside in 1–3 d • Steroids (usually systemic; occ. intrapericardial) only for systemic rheum or autoimmune disorder, uremic, preg., contraindication to NSAID, or refractory idiopathic dis.
Systemic steroids appear to ↑ rate of pericarditis recurrence (
Circ
2008;118:667).
• Avoid anticoagulants • Infectious effusion → pericardial drainage (preferably surgically) + systemic antibiotics • Acute idiopathic effusion self-limited in 70–90% of cases • Recurrent pericarditis (
Circ
2007;115:2739)
risk factors: subacute, lg effusion/tamponade, T >38°C, lack of NSAID response after 7 d treatment: add colchicine 0.5–1 mg bid × 6 mo (
Annals
2011;155:409)
• Recurrent effusion: consider pericardial window (percutaneous vs. surgical)
PERICARDIAL TAMPONADE
Etiology
• Any cause of pericarditis but esp.
malignancy
,
uremia
,
idiopathic
, proximal aortic dissection with rupture, myocardial rupture • Rapidly accumulating effusions most likely to cause tamponade as no time for pericardium to stretch (eg, to ↑ compliance) and accommodate ↑ intrapericardial fluid volume
Pathophysiology (
NEJM
2003;349:684)
• ↑ intrapericardial pressure, compression of heart chambers, ↓ venous return → ↓ CO
• Diastolic pressures ↑ & equalize in all cardiac chambers → minimal flow of blood from RA to RV when TV opens → blunted
y
descent • ↑ ventricular interdependence → pulsus paradoxus (pathologic exaggeration of nl physio)
Inspiration → ↓ intrapericardial & RA pressures → ↑ venous return → ↑ RV size → septal shift to left. Also, ↑ pulmonary vascular compliance → ↓ pulm venous return. Result is ↓ LV filling → ↓
LV stroke volume
& blood pressure.
Clinical manifestations
•
Cardiogenic shock
(hypotension, fatigue)
without pulmonary edema
• Dyspnea (seen in ~85%) may be due to ↑ respiratory drive to augment venous return
Physical exam (
JAMA
2007;297:1810)
•
Beck’s triad
(present in minority of cases):
distant heart sounds
, ↑
JVP
,
hypotension
• ↑ JVP (76%) w/ blunted
y
descent • Reflex tachycardia (77%), hypotension (26%; occasionally hypertensive), cool extremities •
Pulsus paradoxus
(Se 82%, Sp 70%) = ↓ SBP ≥10 mmHg during inspiration
LR 3.3 (5.9 if pulsus >12),
LR 0.03
Ddx = PE, hypovolemia, severe COPD, constriction (~
1
⁄
3
), RV infarct
Can be absent if pre-existing ↑ LVEDP, arrhythmia, severe AI, ASD, regional tamponade
• Distant heart sounds (28%), ± pericardial friction rub (30%) • Tachypnea but clear lungs
Diagnostic studies
• ECG: ↓ voltage (seen in 42%), electrical alternans (20%), ± signs of pericarditis • CXR: ↑ cardiac silhouette (89%) •
Echocardiogram
:effusion
, IVC plethora,
septal shift
with inspiration
diastolic collapse
of RA (Se 85%, Sp 80%) and/or RV (Se <80%, Sp 90%)
respirophasic
Δ
’s in transvalvular velocities
(↑ across TV & ↓ across MV w/ inspir.)
postsurgical tamponade may be localized and not easily visible
• Cardiac cath (right heart and pericardial): elevation (15–30 mmHg) and equalization of
intrapericardial and diastolic pressures (RA, RV, PCWP), blunted
y
descent in RA
↑ in stroke volume postpericardiocentesis = ultimate proof of tamponade
Other books
License to Thrill by Elizabeth Cage
El Talón de Hierro by Jack London
Finding My Highlander by Aleigha Siron
The Girls She Left Behind by Sarah Graves
A Shade of Dragon 3 by Forrest, Bella
A Dangerous Beauty by Sophia Nash
Mrs. Jeffries Speaks Her Mind by Brightwell, Emily
Rebel Obsession by Lynne, Donya
Love notes by Avis Exley