Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (54 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
5.82Mb size Format: txt, pdf, ePub
•UAG → failure of kidneys to secrete NH
4
+ Ddx: distal or hypoaldo RTA, early renal failure
nb, plasma K usually ↓ in distal and ↑ in hypoaldo RTA
• UAG evaluation assumes Pt volume replete (U
Na
>25) & no AG met. acid. (which causesUAG due to excretion of organic anions)
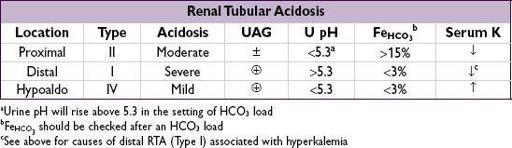
Renal tubular acidoses (RTAs)
(
JASN
2002;13:2160;
Int J Clin Pract
2011;65:350)
•
Proximal
(Type II): ↓ proximal reabsorption of HCO
3
1° (Fanconi’s syndrome = ↓ proximal reabsorption of HCO
3
, PO
4
, glc, amino acids), paraprotein (multiple myeloma, amyloidosis), meds (acetazolamide, heavy metals, ifosfamide), renal transplant, ↓ Vit D, NRTIs
•
Distal
(Type I): defective distal H+ secretion
1°, autoimmune (Sjögren’s, RA), nephrocalcinosis, meds (ampho, Li, ifosfamide); normally a/w ↓ K; if with ↑ K → sickle cell, obstruction, SLE, renal transplant
•
Hypoaldo
(Type IV): ↑ K → ↓ NH
3
synthesis/delivery → ↓ urine acid carrying capacity
↓ renin: diabetic nephropathy, NSAIDs, chronic interstitial nephritis, HIV
normal renin, ↓ aldo synthesis: 1° adrenal disorders, ACEI, ARBs, heparin
↓ response to aldosterone
meds: K-sparing diuretics, TMP-SMX, pentamidine, calcineurin inhibitors
tubulointerstitial disease: sickle cell, SLE, amyloid, diabetes
• Combined (Type III): rarely discussed or clinically relevant, also called juvenile RTA, has distal & proximal features, can be due to carbonic anhydrase II deficiency
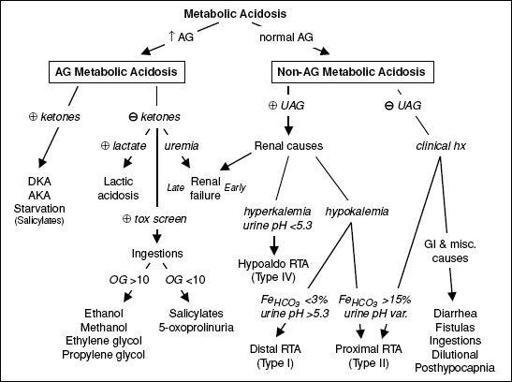
Figure 4-2 Approach to metabolic acidosis
Treatment of severe metabolic acidoses (pH <7.2)
(
Nat Rev Nephol
2012;8:589)
• DKA: insulin & IVF; AKA: dextrose, IVF, replete K, Mg, PO
4
as needed
• Lactic acidosis: treat underlying condition, avoid vasoconstrictors
• Renal failure: hemodialysis
• Methanol & ethylene glycol: early fomepizole, vit. B
6
(ethylene glycol), folate (methanol), hemodialysis (esp. if late presentation) (
NEJM
2009;360:2216)
• Alkali therapy: NaHCO
3
(eg, three 50-mmol amps in 1 L D
5
W) to get serum HCO
3
>8 and pH >7.2 (estimate mmol of HCO
3
needed as 8-[HCO
3
]
serum
× wt × 0.5) side effects: ↑ volume, ↑ Na, ↓ ICa, ↑ P
a
CO
2
(& ∴ intracellular acidosis), overshoot
No proven benefit in lactic acidosis or DKA (
Annals
1986;105:836 & 1990;112:492)
• THAM (proton acceptor) in Pts w/ ↑ P
a
CO
2
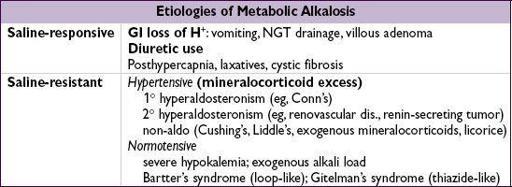
METABOLIC ALKALOSIS
Pathophysiology
• Saline-responsive etiologies require
initiating event
and
maintenance phase
•
Initiating event:
gain of HCO
3
or loss of acid
loss of H
+
from GI tract or kidneys
exogenous alkali
: iatrogenic HCO
3
administration, milk alkali syndrome
contraction alkalosis
: diuresis → excretion of HCO
3
-poor fluid → extracellular fluid “contracts” around fixed amount of HCO
3
→ ↑ HCO
3
concentration
posthypercapnia
: respiratory acidosis → renal compensation with HCO
3
retention; rapid correction of respiratory disorder (eg, with intubation) → transient excess HCO
3
•
Maintenance phase
volume depletion
→ ↑ proximal reabsorption of NaHCO
3
and ↑ aldosterone (see next)
hyperaldosteronism
(either 1° or 2°) → distal Na reabsorption in exchange for K+ and H+ excretion (and consequent HCO
3
retention)
hypokalemia
→ transcellular K+/H+ exchange; intracellular acidosis in renal proximal tubular cells promotes bicarbonate reabsorption and ammoniagenesis
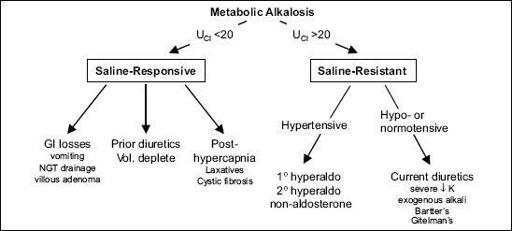
Workup
• Check
volume status
and
U
Cl
U
Cl
<20 mEq/L → saline-responsive
U
Cl
>20 mEq/L → saline-resistant (unless currently receiving diuretics)
(U
Na
unreliable determinant of volume status as alkalemia → ↑ HCO
3
excretion → ↑ Na excretion; negatively charged HCO
3
“drags” Na+ along)
If U
Cl
>20 and volume replete, ✓
blood pressure
Figure 4-3
Approach to metabolic alkalosis
Treatment of severe metabolic alkalosis (pH >7.6)
• If volume depletion: d/c diuretics and correct volume deficit with isotonic saline If cardiopulmonary disease precludes hydration, can use KCl, acetazolamide, HCl • If NGT drainage that cannot be stopped: PPI • Hyperaldosteronism: treat underlying condition
RESPIRATORY ACIDOSIS
Etiologies
•
CNS depression
: sedatives, CNS trauma, O
2
in chronic hypercapnia (↓ hypoxemic drive), central sleep apnea
•
Neuromuscular disorders
: myasthenia gravis, Guillain-Barré, poliomyelitis, ALS, muscular dystrophy, severe hypophosphatemia, high spinal cord injury, drugs (paralytics)
•
Upper airway abnormalities
: acute airway obstruction, laryngospasm, obstructive sleep apnea, esophageal intubation
•
Lower airway abnormalities
: asthma, COPD
Other books
Death Will Help You Leave Him by Zelvin, Elizabeth
Tribulation Road: A Red Hot Treats Story by Colt, Shyla
Turkey Monster Thanksgiving by Anne Warren Smith
Coastal Event Memories by A. G. Kimbrough
Prison Ship by Bowers, Michael
Imprisoned at Werewolf Keep (Werewolf Keep Trilogy) by Glover, Nhys
to Tame a Land (1955) by L'amour, Louis
Stranger in the Mirror [Shades of Heaven] (Soul Change Novel) by Tina Wainscott
The Laws of Attraction by Sherryl Woods
Second Son by Lee Child