Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (97 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
9.74Mb size Format: txt, pdf, ePub
Jod-Basedow effect: iodine load → ↑
synthesis
of T
4
and T
3
in autonomous tissue
• Type 2 = destructive thyroiditis
↑
release
of preformed T
4
& T
3
→ hyperthyroidism → hypothyroidism → recovery
• Doppler U/S: type 1 w/ ↑ thyroid blood flow; type 2 w/ ↓ flow
• Treatment: not absolutely necessary to d/c amio b/c amio ↓ T
4
→ T
3
conversion methimazole for type 1; steroids for type 2 often difficult to distinguish so Rx for both typically initiated (
JCEM
2001;86:3) consider thyroidectomy in severely ill patient
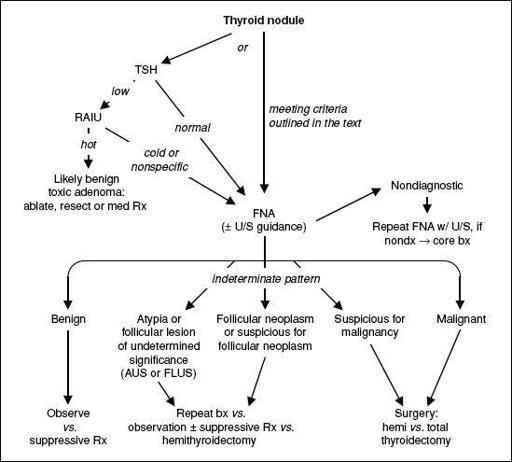
THYROID NODULES
• Prevalence 5–10% (50–60% if screen with U/S), ~5% malignant
• Features associated w/ ↑ risk of malignancy: age <20 or >70 y,, h/o neck XRT, hard and immobile mass, cold nodule on RAIU, large size, worrisome U/S findings (hypoechoic, solid, irregular borders, microcalcifications, central blood flow), cervical LAN
• Features associated w/ benign dx: FHx of autoimmune thyroid disease or goiter, presence of hypothyroidism or hyperthyroidism, nodule tenderness • Screening U/S recommended for those with FHx of MEN2 or medullary thyroid cancer, personal h/o neck XRT, palpable nodules or multinodular goiter • Any evidence of tracheal deviation or compression → ✓ PFTs & refer to surgery
• FNA for nodules >10 mm (>8 mm if irregular borders), microcalcifications or central vasculature; FNA any nodules in Pts with h/o neck XRT or FHx of MEN2 or MTC
• Indeterminate pattern in 15–30% of FNA; gene expression pattern has Se 92% & Sp 52% for malignancy (
NEJM
2012;367:705) • Suppressive Rx w/ high doses of levothyroxine less successful in iodine-sufficient regions • After complete surgical resection of thyroid cancer, RAI is administered (in Pts w/ low-risk thyroid cancer, this practice is controversial) (
Lancet
2013;381:1046 & 1058)
Figure 7-2 Approach to thyroid nodules (
Thyroid
2009;19:1167;
Am J Clin Pathol
2009;132:658)
ADRENAL DISORDERS
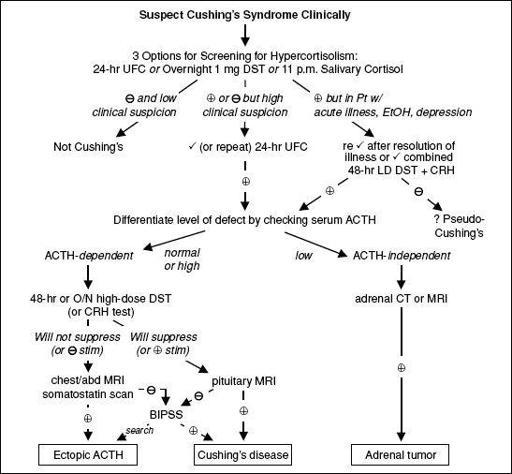
CUSHING’S SYNDROME (HYPERCORTISOLISM)
Definitions
• Cushing’s syndrome = cortisol excess
• Cushing’s disease = Cushing’s syndrome 2° to pituitary ACTH hypersecretion
Etiologies of hypercortisolism
• Most common is iatrogenic Cushing’s syndrome caused by exogenous glucocorticoids
•
Cushing’s disease
(60–70%): pituitary adenoma (usually microadenoma) or hyperplasia •
Adrenal tumor
(15–25%): adenoma or (rarely) carcinoma
•
Ectopic ACTH
(5–10%): SCLC, carcinoid, islet cell tumors, medullary thyroid cancer, pheo
Clinical manifestations
•
Nonspecific:
glucose intolerance or DM, HTN, obesity, oligo-or amenorrhea, osteoporosis •
More specific:
central obesity w/ extremity wasting, dorsocervical fat pads, rounded facies •
Most specific:
spontaneous bruising, proximal myopathy, wide striae, hypokalemia • Other: depression, insomnia, psychosis, impaired cognition, facial plethora, acne, hirsutism, hyperpigmentation (if ↑ ACTH), fungal skin infxns, nephrolithiasis, polyuria
Figure 7-3 Approach to suspected Cushing’s syndrome (
nb, very difficult to diagnose as an inpatient
)
CRH, corticotropin-releasing hormone; DST, dexamethasone suppression test; UFC, urinary free cortisol Overnight 1 mg DST = give 1 mg at 11 p.m.; ✓ 8 a.m. serum cortisol (suppression if <1.8 µg/dL); 1–2% false(primarily used to evaluate subclinical Cushing’s in adrenal “incidentalomas”) (
JCEM
2008;93:1526) 11 pm salivary cortisol = abnl if level ↑; 24-h UFC = abnl if level ↑, > 4× ULN virtually diagnostic 48-h LD DST + CRH = 0.5 mg q6h × 2 d, then IV CRH 2 h later; ✓ serum cortisol 15 min later (= >1.4 µg/dL) 48-h LD DST = 0.5 mg q6h × 2 d; ✓ 24-h UFC at base. & during last 24 h of dex (suppress if <10% of base) 48-h HD DST = 2 mg q6h × 2 d; ✓ 24-h UFC as per LD DST
O/N HD DST = 8 mg at 11 p.m.; ✓ 9 a.m. serum cortisol (suppression if <32% of baseline) CRH test = 1 µg/kg IV; ✓ cortisol and ACTH (stim if > 35% ↑ in ACTH or >20% ↑ in cortisol above baseline) BIPSS, bilat. inferior petrosal sinus vein sampling; ✓ petrosal:peripheral ACTH ratio (
= 2 basal, >3 after CRH) (J Clin Endocrinol Metab 2008;93:1526)
Treatment of Cushing’s syndrome
• Surgical resection of pituitary adenoma, adrenal tumor or ectopic ACTH-secreting tumor • If transsphenoidal surgery (TSS) not successful → pituitary XRT, medical adrenalectomy w/ mitotane, or bilat surgical adrenalectomy; ketoconazole (± metyrapone) to ↓ cortisol • Glucocorticoid replacement therapy × 6–36 mo after TSS (lifelong glucocorticoid + mineralocorticoid replacement if medical or surgical adrenalectomy)
HYPERALDOSTERONISM
Etiologies
•
Primary
(adrenal disorders, renin independent increase in aldosterone) adrenal hyperplasia (60%), adenoma (
Conn’s syndrome
, 35%), carcinoma (5%) glucocorticoid-remediable aldosteronism (GRA; ACTH-dep. rearranged promoter)
•
Secondary
(extra-adrenal disorders, ↑ aldosterone is renin dependent)
Primary reninism: renin-secreting tumor (rare)
Secondary reninism
renovascular disease: RAS, malignant hypertension
edematous states w/ ↓ effective arterial volume: CHF, cirrhosis, nephrotic syndrome
hypovolemia, diuretics, T2D, Bartter’s (defective Na/K/2Cl transporterreceiving loop diuretic), Gitelman’s (defective renal Na/Cl transporter
receiving thiazide diuretic)
Other books
The Death Strain by Nick Carter
Brady's Hellion by Linda Wisdom
Shadow Tag (The Ray Schiller Series - Book 2) by Doering, Marjorie
Words of Love by Hazel Hunter
Pretty Sly by Elisa Ludwig
The Case Against Owen Williams by Allan Donaldson
Get-Together Summer by Lotus Oakes
Faded Cotton (Erotic Romance) by Lara Sweety
Wildflower by Prudence MacLeod
The Skeleton Box by Bryan Gruley