Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (58 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
2.88Mb size Format: txt, pdf, ePub
Contrast-induced acute kidney injury (CIAKI)
• Risk factors: CKD, DM, CHF, age, hypotension, ↑ contrast volume (
JACC
2004;44:1393) • Clinical: Cr ↑ 25% or 0.5 mg/dL w/in 48 h, peaks in 3–5 d, resolves in 7–10 d • Prevention (
NEJM
2006;354:379;
JAMA
2006;295:2765;
KI Suppl
2012;2:69)
Isotonic IV fluids
(unless contraindic, eg, CHF): 3 mL/kg/h × 1 h before, 1 mL/kg/h × 6 h after (
JAMA
2004;291:2328); NaHCO
3
? more effective than NaCl (
Annals
2009;151:631)
Hold ACEI
/
ARB
(
AJKD
2012;60:576),
NSAIDs
,
diuretics
N-acetylcysteine
1200 mg PO bid on day prior to & day of contrast; safe & ∴ reasonable in high-risk Pts, but benefit remains unclear (
JACC CV Interv
2009;2:1116;
Circ
2011;124:1250) Minimize contrast volume and consider iso-osmolar contrast (
JACC
2006;48:692) ? high-dose statin (
Circ
2012;126:3008) No proven benefit to Ppx RRT in addition to above, may be harmful (
Am J Med
2012;125:66)
• Gadolinium: can cause AKI in stage IV CKD (
Neph Dial Trans
2006;21:697), no effective Ppx Nephrogenic systemic fibrosis: fibrosis of skin, joints, eyes, and internal organs ~2–4 wk post exposure in Pts w/ mod-severe CKD (
JACC
2009;53:1621). ? role of postgado HD (
Radiat Med
2006;24:445). Rx is ↑ renal function, physical therapy. Can be irreversible.
Treatment
• Treat underlying disorder (see relevant sections); ? steroids if AIN (
KI
2008;73:940) • Prerenal: Isotonic IVFalb (
NEJM
2004;350:22), HES (starch) nephrotoxic (
NEJM
2012;367:124) • Avoid nephrotoxic insults; review dosing of renally cleared drugs • Optimize hemodynamics (both MAP & CO); may take 1–2 wk to recover from ATN
• Watch for and correct volume overload, electrolyte (↑ K, ↑ PO
4
), & acid/base status • If obstruction is diagnosed and relieved, watch for:
Hypotonic diuresis (2° buildup of BUN, tubular damage); Rx w/ IVF (eg,
1
/
2
NS)
Hemorrhagic cystitis (rapid Δ in size of bladder vessels); avoid by decompressing slowly
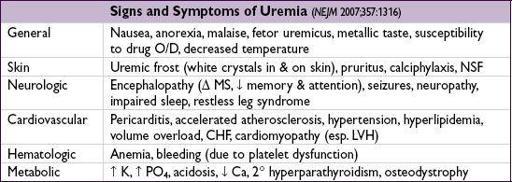
• Indications for urgent dialysis (when condition refractory to conventional therapy)
A
cid-base disturbance: acidemia
E
lectrolyte disorder: generally hyperkalemia; occasionally hypercalcemia, tumor lysis
I
ntoxication: methanol, ethylene glycol, lithium, salicylates (
Kid Int
2009;75:1349)
O
verload of volume (CHF)
U
remia: pericarditis, encephalopathy, bleeding
•
No
benefit to dopamine (
Annals
2005;142:510), diuretics (
JAMA
2002;288:2547), or mannitol
CHRONIC KIDNEY DISEASE (CKD)
Definition and etiologies
(
Lancet
2012;379:165)
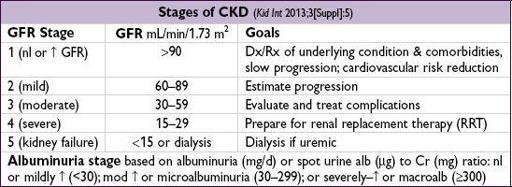
• ≥3 mo of
reduced GFR
(<60)
and
/
or
kidney damage
(path, markers, imaging)
• Prevalence 13% in U.S.; Cr poor estimate of GFR; ∴ use prediction equation, eg, MDRD or CKD-EPI:
www.kidney.org/professionals/KDOQI/gfr_calculator.cfm
nb, equation may underestimate GFR in Pts w/ normal renal fxn, esp MDRD
• Etiologies: DM (45%), HTN/RAS (27%), glomerular (10%), interstitial (5%), PKD (2%) (
NEJM
2008;359:1477), congenital, drugs, myeloma, progression of AKI (
JAMA
2009;302:1179)
• Presence and degree of albuminuria a/w worse outcomes independent of GFR
• Rates of all-cause mortality and CV events increase with each stage of CKD and are significantly higher than the rate of progression to kidney failure (
NEJM
2004;351:1296)
Treatment
(
Annals
2009;150:ITC2-1;
NEJM
2010;362:57)
•
General
: nephrology referral when GFR <30 and access planning (avoid subclavian lines; preserve an arm for access by avoiding blood draws, BP measurements, IVs); Rx CV risk factors (eg, smoking, LDL-C;
Lancet
2011;377:2181), vaccines (flu, PNA, HBV)
•
Dietary restrictions
: Na (if HTN), K (if oliguric or hyperkalemic), PO
4
, ? moderate protein restriction, strict glc control in DM
•
BP Control
: goal <130/80, start with ACEI (or ARB), effective in DM & nondiabetic CKD (
NEJM
2004;351:1952); likely no benefit of ACEI + ARB (
BMJ
2013;346:f360). For outPts, ✓ Cr & K in 1–2 wk, d/c if Cr ↑ 30% or K >5.4 (after dietary Δ & loop diuretic).
•
Metabolic acidosis
: sodium bicarbonate or sodium citrate if low HCO
3
(
JASN
2009;20:2075)
•
Anemia
: goal Hb ~10 g/dL, worse outcomes if higher (
NEJM
2006;355:2085 & 2009;361:2019) epoetin (start 80–120 U/kg SC, divided 3×/wk) or darbepoetin (0.45 µg/kg q wk) iron supplementation to keep transferrin sat >20% (often given IV in HD Pts)
•
Uremic bleeding
: desmopressin (dDAVP) 0.3 µg/kg IV or 3 µg/kg intranasally
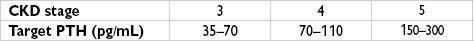
•
2
°
Hyperparathyroidism
: ↑ PO
4
, ↓ Ca, ↓ calcitriol → ↑ PTH → renal osteodystrophy
phosphorus binders (
take with meals!
) (
NEJM
2010;362:1312)
if ↑ PO
4
and ↓ Ca → calcium acetate (PhosLo) or calcium carbonate
if refractory ↑ PO
4
or in setting of ↑ Ca → sevelamer (Renagel), lanthanum (Fosrenol)
if severe ↑ PO
4
→ aluminum hydroxide (Amphojel),
short-term use only
vit. Δ or analogue (paricalcitol) if 25-(OH)D <30, stop if ↑ Ca (
AJKD
2009;53:408) calcitriol or paricalcitol if Ca-PO
4
product <55 (? ↑ survival in HD Pts,
NEJM
2003;349:446) cinacalcet (parathyroid calcium-sensing receptor agonist) if PTH remains elevated despite phosphorus binders ± vit. Δ analogue (
NEJM
2004;350:1516;
NDT
2011;26:1327) parathyroidectomy
•
Consider transplant evaluation
DIURESIS
General considerations
• Increases Na excretion for treatment of HTN or edema in CHF, renal failure, and cirrhosis • Daily wt most effective method of documenting successful diuresis
Loop diuretics
(
NEJM
1998;339:387)
•
Drugs
: furosemide (Lasix), torsemide, bumetanide (Bumex), ethacrynic acid •
Mechanism
: inhibit Na-K-2Cl transporter in thick ascending limb (ThAL) Transient, immediate venodilation may aid in pulmonary congestion (
NEJM
1973;288:1087) Response is fxn of amt of drug excreted; ∴ ↑ dose needed in renal insufficiency, CHF Sigmoidal dose response curve; ∴ ↑ dose until induce diuresis, ↑↑ dose beyond that point yields diminishing returns compared with ↑ frequency of dosing •
Dosing
: PO bioavailability of furosemide ~50%, ∴ IV dose ~2× as potent as PO dose torsemide & bumetanide ~90% bioavailability; use ethacrynic acid if sulfa allergy 40 mg furosemide PO20 mg furosemide IV
20 mg torsemide PO
1 mg bumetanide dose furosemide bid-qid; qd dosing can lead to initial diuresis → antinatriuresis Continuous vs. bolus IV: similar results in acute CHF (
NEJM
2011;364:797)
Other books
Learning to Waltz by Reid, Kerryn
Wet Dreamz by Bobbi Romans
Margaret St. Clair by The Best of Margaret St. Clair
The Case of the Sin City Sister by Lynne Hinton
The Turning Season by Sharon Shinn
Guardian Bride by Lauri Robinson
Cupid's Cupcake by Sinclair, Ivy
Wild Boy by Mary Losure
The Going Rate by John Brady
Beautiful Lies by Jessica Warman