The Washington Manual Internship Survival Guide (25 page)
Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine

•
PID often requires inpatient treatment, but can sometimes be treated on an outpatient basis if specific criteria are met. Either form of treatment requires close follow-up with an OB/GYN.
•
If inadequately treated, PID can lead to infertility, chronic pelvic pain, sepsis, and even death.
•
If PID is suspected, an OB/GYN consult should be obtained. For treatment guidelines, see
www.cdc.gov
.
Ectopic Pregnancy
•
Pertinent information:
Notify the OB/GYN team immediately if you suspect ectopic pregnancy
. A ruptured ectopic pregnancy is a surgical emergency.
•
History:
• Last menstrual period.
• Symptoms: Missed menstrual period, abdominal pain, and/or vaginal spotting.
• Possible risk factors for ectopic pregnancy: Prior ectopic pregnancy, history of tubal ligation or other tubal surgery, history of prior gynecologic infection or PID.
•
Physical exam:
• Vital signs, include orthostatics.
• General: Note degree of pallor, weakness, responsiveness, pain.
• Cardiovascular: Note presence of tachycardia, quality of peripheral pulses.
• Abdomen: may palpate presence of a mass, rebound or guarding (signs of peritonitis), abdominal distension.
• Pelvic exam: may or may not see bleeding via cervical os, cervical dilation, slightly enlarged uterus, palpable adnexal mass.
•
Labs: CBC, T&S, qualitative urine hCG. If positive urine hCG, obtain a
quantitative
serum ß-hCG.
•
Imaging: Abdominal and pelvic ultrasound (transvaginal) to determine location of pregnancy, gestational age, and fetal heart motion.
•
Treatment:
• IV access and fluid resuscitation (have cross-matched blood available).
• Removal of the ectopic pregnancy: Medical (methotrexate) versus surgical management will be based on characteristics of the ectopic, stability of the patient, and patient preference. The OB/GYN consult team will determine the mode of treatment.
Vaginal Bleeding
•
Pertinent information: Severity of bleeding will dictate the extent of your workup prior to calling a consult. See
Figure 21-2
for the most common pathologic etiologies of vaginal bleeding. Vaginitis and cervicitis also cause vaginal spotting and can occur in any of these age groups.
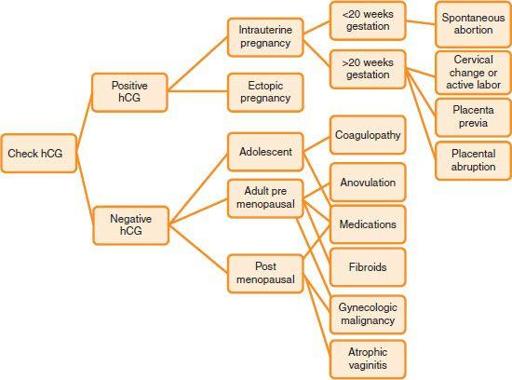
Figure 21-2.
Approach to vaginal bleeding.
•
History: Note date of last normal menstrual period; the frequency, quantity, and duration of the bleeding; whether there is a history of bleeding disorders; and whether the patient is on hormones, contraception, or anticoagulants. Inquire whether she has ever had a history of any gynecologic problems in the past and whether she has a family history of any gynecologic problems, including gynecologic cancer.
Suspect malignancy in any postmenopausal patient with vaginal bleeding
.
•
Physical exam: An abdominal exam, speculum exam, and pelvic exam should be performed in order to determine the source and extent of bleeding. Rule out urologic and GI sources of bleeding: spread the labia to inspect the urethra, send a macro/micro urinalysis (straight cath specimen), and perform a digital rectal exam/guaiac. Vaginal bleeding may be coming from the uterus via the cervical os, the cervix itself, or the vaginal walls.
•
Labs: CBC, T&S, PT, PTT, INR, hCG, TSH, prolactin.
•
Imaging: Abdominopelvic imaging (usually ultrasound) to characterize pregnancy status and anatomic causes of bleeding (fibroids, polyps, ovarian masses, endometrial stripe thickness).
•
Pathologic specimens:
• OB/GYN will perform pap and endometrial sampling if indicated.
• Postmenopausal women and women with chronic anovulation, obesity, or age greater than 35 should all have endometrial sampling. These women are at high risk for hyperplasia and malignancy.
•
Treatment:
• IV access, fluid resuscitation, transfusion as needed.
• Strict I/Os, pad counts.
• Consult OB/GYN, as treatment will depend upon etiology.
Pelvic Mass
•
Pertinent information: Call an OB/GYN consult immediately if you suspect ovarian torsion!
Ovarian torsion is a surgical emergency
, and prompt surgical treatment could enable a young woman to keep her ovary. Ovarian torsion is clinically diagnosed. It may present with constant or intermittent severe abdominal pain, a tender pelvic mass, and low-grade temperatures. Pelvic ultrasound may demonstrate one enlarged ovary.
•
History: Obtain a thorough OB/GYN history.
•
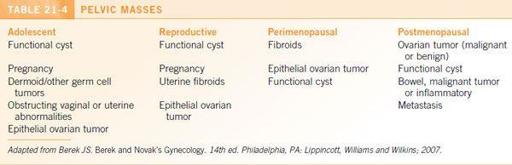
Differential diagnosis: Pelvic masses may be gynecologic in origin or may arise from the urinary tract or bowel. Age is an important determinant of the likelihood of malignancy.
Table 21-4
outlines the most common causes of pelvic masses for each age group. Additionally, an infectious cause (e.g., tubo-ovarian abscess) can occur in association with PID.
•
Physical exam: A gynecologic exam should be performed. Ascites or pleural effusion heightens the suspicion for ovarian cancer.
•
Labs:
• CBC and hCG (in reproductive age women).
• Tumor markers: Obtain in consultation with OB/GYN.
•
Imaging: The OB/GYN consult team will help guide imaging. Transvaginal pelvic ultrasound will help to delineate the origin and internal features of the mass. If malignancy is suspected or confirmed, further imaging (CT, MRI) may be indicated to determine the extent of disease. A barium enema or colonoscopy will help to exclude a gastrointestinal etiology.
•
Treatment: Varies greatly, depending on etiology.
OPHTHALMOLOGY
The Ophthalmologic History and Examination
•
Basic ophthalmic history:
• Chief complaint: Course/extent of vision loss, unilateral/bilateral symptoms, central/peripheral visual symptoms, constant/intermittent symptoms, presence of pain.
• Prior ophthalmic history: Known ophthalmic conditions, prior eye surgery or trauma, contact lens/eye medication use, and relevant past medical/family history.
•
Basic ophthalmic exam:
•
Visual acuity (extremely important)
: acuity for each eye (have the patient wear his/her glasses). If no vision chart is available, have the patient attempt to read your name badge, the newspaper, or signs around the room.
• Pupillary exam: Are the pupils/iris visible through the cornea? Are they round and equal in size? Do they react to light?
• Motility exam: Determine whether the eyes are aligned in primary gaze; test ocular motility and determine if nystagmus is present.
• Visual field exam: Test each individual eye (start with the eye with better vision); determine whether the patient can count fingers at the edges of central vision.
• External exam: Are the eyes proptotic? Is eyelid position normal? Is the eye red?
• Fundus exam. Determine whether there is a red reflex. Look for optic nerve swelling, retinal hemorrhage, or retinal detachment. It is often helpful to communicate the level of confidence of your fundus exam to the consultant.
Injury
Trauma with Possible Ruptured Globe
•
Ocular emergency: call a consult immediately!
•
Pertinent information: Age, PMH including ocular history, allergies, current medications including ocular medications, specific ocular complaints, history of events preceding trauma, specific chemicals or items involved, any history of possible foreign body (e.g., hammering on metal).
•
Typical symptoms: Pain, decreased vision, history of trauma.
•
Physical exam findings suggestive of a ruptured globe: 360° subconjunctival hemorrhage, full-thickness corneal or scleral laceration, peaked or irregular pupil, exposed intraocular contents, hyphema (bleeding in the anterior chamber).
•
Treatment:
• Place a shield over the involved eye; do not press on eye or touch ocular contents.
• NPO (determine last meal).
• IV antibiotics: Cefazolin or vancomycin 1 g IV immediately; also give fluoroquinolone (e.g., ciprofloxacin or moxifloxacin PO or IV).
• Administer tetanus toxoid as needed.
• Antiemetic as needed to prevent Valsalva.
• Orbital CT scan (axial and coronal).
•
Surgical repair as soon as possible
.
•
Clinical pearl: In trauma with eyelid laceration, do not try to repair the laceration. Allow ophthalmologist to assess extent.
Acute Chemical Splash
•
Ocular emergency: Begin irrigation, and then call a consult immediately!
•
Pertinent information: Age, PMH including ocular history, allergies, current medications including ocular medications, specific ocular complaints, history of events, specific chemicals and amounts involved, time/duration of contact, irrigation at scene.
•
Symptoms: Possible pain, blurry vision, foreign body sensation, tearing, photophobia.
•
Physical exam:
• Mild to moderate splash: Sloughing of entire epithelium, hyperemia, mild chemosis (edema of bulbar conjunctiva), eyelid edema, first- or second-degree periocular skin burns.
• Moderate to severe: Pronounced chemosis, perilimbal (at the junction of cornea and sclera) blanching, corneal edema or opacification, anterior chamber reaction/no view of the anterior chamber or iris, increased intraocular pressure, second- or third-degree burns.
•
Workup: Slit-lamp exam, evert eyelids; check pH, intraocular pressure.
•
Immediate treatment (prior to contacting consult service):
•
Copious irrigation
with 1 L of any available irrigant (e.g., NS, 1/2 NS, or LR), and keep irrigating until you talk with the consultant.
• May give 1 to 2 drops of topical anesthetic.
• Do not use acid or alkali to neutralize splash.
• Check pH 5 minutes after irrigation; continue irrigation until pH is neutral (i.e., 7).
•
Treatment
after irrigation
(ideally instituted by ophthalmologist):
• Debride necrotic tissue.
• Topical antibiotic ointment: bacitracin/polymyxin, erythromycin, or ciprofloxacin ophthalmic qid.
• Additional treatments including cycloplegia, the use of topical steroids, and intraocular pressure control should be instituted by an ophthalmologist with plans for frequent follow-up.
Corneal Ulcer
•
This is an emergency; call a consult immediately!
•
Pertinent information: Age, past ocular history (previous ulcers or herpetic infections?), history leading up to event (recent trauma or contact lens use).