Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine
The Washington Manual Internship Survival Guide (26 page)

•
Symptoms: pain, photophobia, decreased vision, with or without discharge.
•
Physical exam: Focal corneal opacity and overlying epithelial defect (abrasion), anterior chamber reaction, with or without hypopyon (white blood cells layering out in anterior chamber), eyelid edema, lagophthalmos (incomplete eyelid closure).
•
Workup: Routine cultures taken of corneal scrapings (done by ophthalmologist), includes gram stain, KOH prep, fungal culture.
•
Treatment:
•
Moxifloxacin
drops q1-4h and
cycloplegia
with scopolamine 0.25% tid.
• If ulcer is severe, patient will be admitted and given topical fortified antibiotic drops.
• Daily ophthalmology follow-up.
•
Clinical pearls: Contact lens wearers are at much higher risk. Bacteria, fungi, HSV, and
Acanthamoeba
are all possible causes. Inpatients who cannot close their eyes fully are at increased risk for exposure keratopathy and corneal ulcers. Frequent lubrication, use of a moisture chamber, or tarsorrhaphy (performed by an ophthalmologist) can help avoid further corneal damage.
Corneal Abrasion or Foreign Body
•
This is usually not an emergency, but consult if in doubt.
•
Pertinent information: Age, past ocular history, history of events leading up to event, occupational history (i.e., grinding, drilling, trauma), contact lens use, type of foreign body.
•
Symptoms: Acute pain, tearing, photophobia, foreign body sensation.
•
Workup:
• Blue light or slit-lamp exam with fluorescein to detect epithelial defect (seen as green fluorescent spot).
• Look for foreign body or rust ring.
• Measure and record dimension of defect.
• Evert eyelids to look for hidden foreign bodies.
• Look for associated corneal ulcers (white opacity seen before fluorescein instilled).
•
Treatment:
•
Remove foreign body
(preferably by an ophthalmologist).
• Non-contact lens wearers: Treat with
bacitracin/polymyxin or erythromycin
ointment q2-4h or polymyxin B/trimethoprim drops tid.
• Contact lens wearers:
Moxifloxacin drops qid or tobramycin or ciprofloxacin
ointment q2-4h. No contact lens use until cleared by an ophthalmologist.
•
Cycloplegi
a with cyclopentolate 1% tid if any significant photophobia.
• Follow-up next day with an ophthalmologist and follow-up as needed thereafter.
•
Clinical pearls: If there is any chance of penetrating injury, call a consult immediately.
Painless Acute Vision Loss
Central Retinal Artery Occlusion
•
Ocular emergency: call a consult stat!
Like a CVA, “time is vision!”
•
Pertinent information: Age, PMH/PSH/ocular history, allergies, current meds including ocular meds, specific ocular complaints, history of preceding event, vision loss.
•
Symptoms: Painless, unilateral, acute loss of vision, prior history of amaurosis fugax (painless, temporary, uniocular vision loss).
•
Physical exam: Whitening of the retina with a “cherry red” spot in the center of the macula, afferent pupillary defect
(Marcus Gunn pupil), narrowed arterioles, occasionally arteriolar emboli/plaque visible.
•
Workup: ESR in patients over 50 years of age, fasting blood sugar, CBC, PT/PTT; in younger patients, also check ANA, RF, FTA-ABS, SPEP, sickle cell test, and antiphospholipid antibodies. Check blood pressure. Patient may need carotid Doppler and cardiac echo.
•
Treatment:
• Call an ophthalmologist! Permanent visual loss likely after 90 to 120 minutes.
• Ocular massage: Have patient close eyes; apply pressure to the globe for 5 to 15 seconds, then release. Repeat several times.
•
Clinical pearls:
• Ask about symptoms of giant cell arteritis and check ESR in all patients over 50 years of age.
• Etiologies include embolus (carotid or cardiac), thrombosis, giant cell arteritis, collagen vascular disease, hypercoagulable states, and rare causes (i.e., migraine, Behçet’s disease, syphilis).
Retinal Detachment
•
Ocular urgency: call a consult.
•
Pertinent information: Age, PMH/PSH/ocular history, allergies, current meds, specific complaints, history of preceding trauma or surgery.
•
Symptoms: Painless unilateral decreased vision with associated flashes and floaters, curtain or veil across vision, relative visual field defect.
•
Physical exam: Typically a “white and quiet” appearing eye— externally looks normal, usually no afferent pupillary defect unless a large retinal detachment. Fundus exam reveals a white, billowing, or wrinkled retina.
•
Workup: Slit-lamp exam and dilated fundus exam.
•
Treatment:
•
No acute intervention.
• Low-level activity.
• Needs a retina specialist evaluation.
•
Clinical pearls: Risk factors include recent eye surgery, ocular trauma, high myopia, and a retinal detachment in contralateral eye. A peripheral retinal tear or hole may present with only flashes or floaters and no change in vision. These still require urgent ophthalmologic intervention.
Painful Acute Vision Loss
Acute Angle-Closure Glaucoma
•
Ocular emergency: call a consult immediately!
•
Pertinent information: Age, PMH/PSH/ocular history, allergies, current meds including ocular meds, specific ocular complaints, family history, recent surgery, recent laser surgery, cardiovascular/pulmonary status, electrolyte/renal status.
•
Symptoms: Severe pain, blurry vision, colored halos around lights, frontal headache, nausea/vomiting.
•
Physical exam: Conjunctival injection; fixed, mid-dilated pupil (usually in one eye); shallow anterior chamber; acutely elevated intraocular pressure (40s or above).
•
Workup: Slit-lamp exam, measure intraocular pressure.
•
Treatment:
• In the acute setting manage the patient’s pain and nausea as needed.
• Medical treatment involves ophthalmic drops and systemic medications to decrease intraocular pressure and medications to manage associated inflammation—consult ophthalmology first.
• Definitive (laser) treatment by ophthalmologist.
•
Clinical pearls: Be aware of patient’s cardiovascular and pulmonary status; evaluate electrolyte/renal status before starting systemic medications for ocular pressure control. Etiology can be from an anatomic pupillary block, neovascular, anterior displacement of lens-iris diaphragm (i.e., choroidal effusion, tumor), malignant glaucoma, medications (i.e., mydriatics, anticholinergics).
Papilledema/Optic Nerve Swelling
•
Emergency: Call a consult immediately!
•
Pertinent information: Age, PMH/PSH/ocular history, allergies, current meds including ocular meds, specific ocular complaints.
•
Symptoms: Transient vision loss (“gray-outs”), headache, nausea/vomiting, diplopia, visual field defects, pain with eye movement.
•
Physical exam: Unilateral/bilateral swollen, hyperemic discs; blurring of disc margins; obscuration of vessels; can have normal or abnormal papillary responses and color vision (can have sixth nerve palsy from increased ICP).
•
Workup: Check BP; careful ocular exam (pupils, color vision, exam of fundus); urgent orbital and head CT. Consider LP (after head CT), CBC, TSH, ESR. Consider a neurology consult.
•
Treatment:
Treat underlying cause.
•
Clinical pearls: Etiologies you may see on a medical service are vast and include pseudotumor cerebri, subdural/subarachnoid hemorrhage, AVM or sagittal sinus thrombosis, intracranial tumors, brain abscess, meningitis/encephalitis, hydrocephalus, malignant HTN, uveitis, infiltrative disease (i.e., sarcoid, TB, syphilis), ischemic optic neuropathy (i.e., giant cell arteritis), central retinal vein occlusion, papillitis (i.e., multiple sclerosis/optic neuritis, diabetic eye disease). It is often helpful to communicate the level of confidence of your fundus exam to the consultant.
Infection
Endophthalmitis
•
Ocular emergency: Call a consult immediately!
•
Pertinent information: Age, PMH/PSH/ocular history, allergies, current meds including ocular meds, history of ocular surgery or trauma.
•
Symptoms: Unilateral painful eye, decreased vision.
•
Physical exam: Moderate injection, hypopyon (pus behind the cornea), poor red reflex or view to the back of the eye.
•
Treatment:
• Emergent ophthalmologic evaluation.
• Admission.
•
May need culture and injected antibiotics
.
•
Clinical pearls: A diagnosis of endophthalmitis must be considered first in any patient with recent ocular surgery!
Herpes Zoster Virus
•
This is not an ocular emergency but urgent referral to an ophthalmologist is strongly recommended.
•
Pertinent information: Age, PMH, ocular history, immunocompromised/AIDS.
•
History: Skin rash and discomfort, blurred vision, eye pain, red eye.
•
Physical exam: Skin vesicles in dermatomal distribution respecting the midline (Hutchinson sign, if rash involves the tip of the nose, high chance of eye being involved), conjunctivitis, uveitis, scleritis, cranial nerve palsy.
•
Treatment:
• If younger than 40 years, evaluate for immunosuppression.
•
Oral antiviral
(e.g., acyclovir 800 mg PO 5 times a day) for 7 to 10 days.
• Erythromycin ointment to skin lesions bid.
• Artificial tears or erythromycin ophthalmic ointment to eye as needed.
• Follow-up with ophthalmologist.
The Red Eye
Conjunctivitis
•
This is not an emergency (
Figure 21-3
).
•
Pertinent information: Age, possible contacts (1 to 3 weeks prior to onset of symptoms), past ocular history, allergies or previous history of allergic conjunctivitis; make sure there is no pain involved for allergic and viral conjunctivitis.
•
Symptoms:
• Viral: Unilateral red eye, possible associated URI symptoms, mild itching, morning crusting or discharge.
• Allergic: Bilateral itching, mild redness, watery discharge.
• Bacterial: Acute purulent discharge, eyelid edema, decreased vision.
•
Physical exam:
• Viral: Conjunctival injection, crusting, follicles.
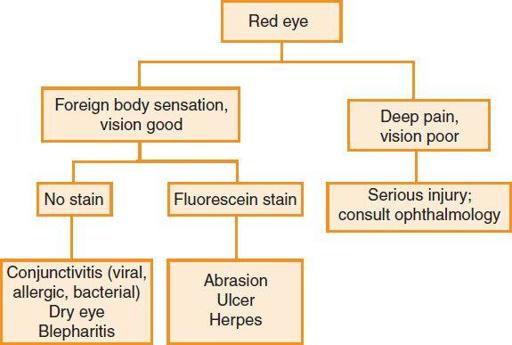
Figure 21-3.
Algorithm for red eye.
• Allergic: Lid swelling, chemosis, papillae.
• Bacterial: Purulent discharge.
•
Workup for bacterial: Gram stain and culture for
Staphylococcus
,
Streptococcus
,
H. flu
,
N. gonorrhoeae.
•
Treatment:
• Viral:
▪ No specific medical treatment necessary, self-limited illness.
▪ Symptomatic treatment with cool compresses or artificial tears.
▪ Naphazoline may be prescribed tid × 7 days.
▪ Wash hands, towels, pillowcases. Use separate towels. No contact lens use until asymptomatic for at least 7 days.
▪ Avoid close contact (especially rubbing eyes and touching others) without washing hands first.
