The Washington Manual Internship Survival Guide (33 page)
Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine

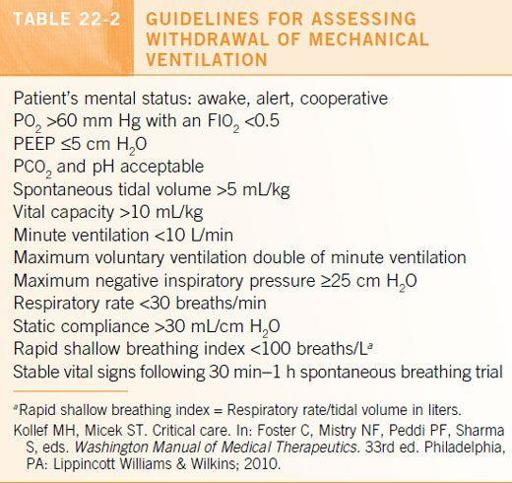
The method of weaning is not as relevant as knowing the appropriate time to wean. See
Table 22-2
.
ICU SEDATION/PARALYSIS
•
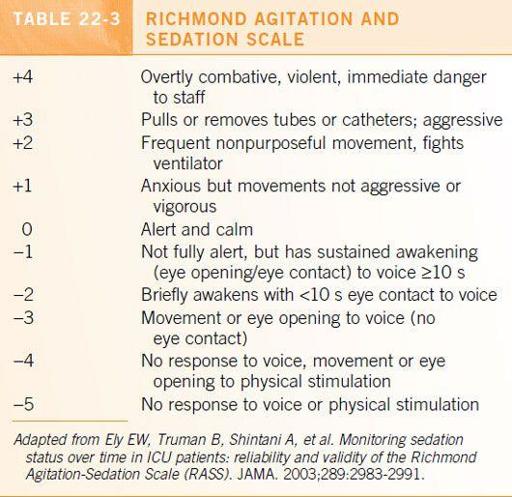
Ventilated patients generally require sedation. This is usually achieved through continuous IV infusion of sedatives. See
Table 22-3
.
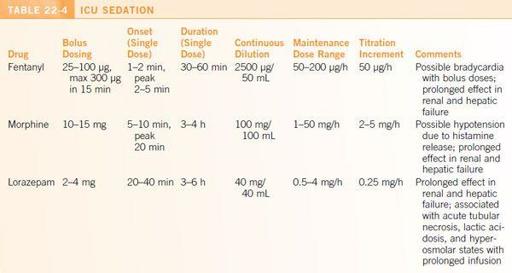
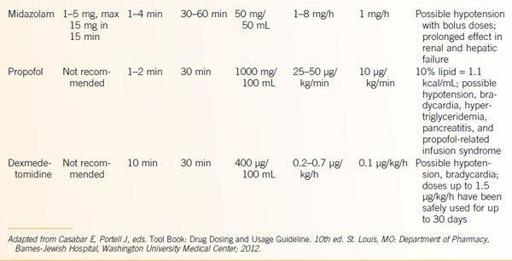
•
Achieve the desired level of sedation with boluses before starting a continuous infusion. Specify the desired level of sedation (
Table 22-4
). If the patient becomes agitated, rebolus to desired level of sedation and then make small incremental changes in the drip rate.
•
Titrate to minimum effective dose and
reassess the need for continuous sedation daily
.
•
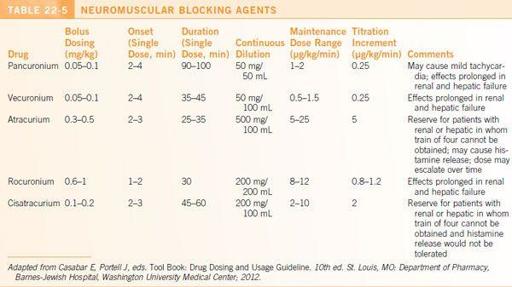
Consider adding paralytics (
Table 22-5
) for patients with very poor oxygenation or if patient–ventilator desynchronization persists despite adequate sedation causing difficulty with ventilation.
Ensure the patient is completely sedated before adding paralytics.
•
The degree of paralysis is usually monitored by peripheral nerve stimulation and the train-of-four method. Complete paralysis is unnecessary for many patients.
•
Paralysis should be discontinued daily to determine the continuing need for paralysis and to assess for adequate sedation
.
CARDIAC PARAMETERS
•
Normal cardiac output: 5 ± 1 L/min
•
Normal cardiac index: 3 ± 0.54 min/m
2
•
Normal filling pressures:
• Right atrial pressure: 0–8 mm Hg
• Right ventricular pressure: 5–30/0–8 mm Hg
• Pulmonary artery pressure: 15–30/3–12 mm Hg
• Pulmonary wedge pressure: 3–12 mm Hg
SHOCK
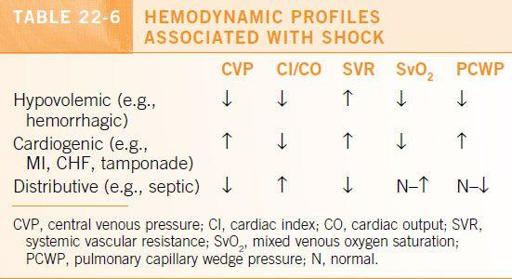
Hemodynamic Profiles Associated with Shock
The hemodynamic parameters associated with the major forms of shock are presented in
Table 22-6
.
Treatment of Shock
•
Determine the type of shock you are dealing with.
•
Fluid resuscitation
is vital, especially for hypovolemic shock. Crystalloid (normal saline or lactated Ringer’s) should be started immediately. For hemorrhagic shock, blood products should be administered.
•
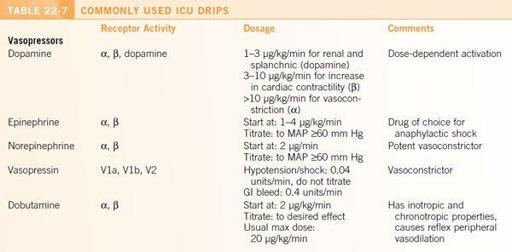
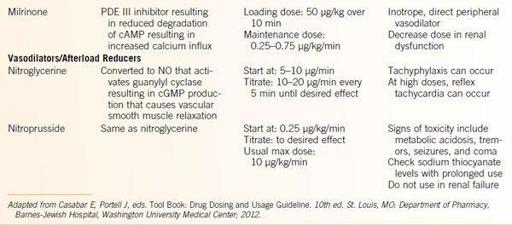
Use of
vasopressors and/or inotropes
may be necessary. Vasoactive agents are generally titrated to a mean arterial pressure of ≥60 to 65 mmHg. Afterload reduction may be helpful in cardiogenic shock. See
Table 22-7
for dosages.
DRIPS
Other intravenous drips commonly used in the ICU are presented in
Table 22-7
.
SUGGESTIONS FOR PROPHYLAXIS
•
DVT: see DVT Prophylaxis section in
Chapter 10
.
•
GI: see GI Prophylaxis section in
Chapter 10
.
•
Decubitus ulcers: turning patient several times a day, vigilant skin care, egg crate mattress, flotation bed, and ensuring adequate nutrition.
•
Deconditioning: physical therapy and nutritional support.
•
Aspiration precautions: elevate head of the bed >30° and adequate suctioning.
•
Seizure or fall precautions: as appropriate.
•
Infection: maintain oral hygiene, keep track of all lines (peripheral IV, central line, NG tube, feeding tubes, Foley catheters), and remove as soon as no longer needed. Target or discontinue antibiotic therapy per guidelines to reduce induction of resistance and development of
Clostridium difficile
colitis.
•
Follow isolation (respiratory or contact) precautions at all times and practice scrupulous hand hygiene.
TOTAL PARENTERAL NUTRITION
•
Consider this option if the GI tract is unusable for at least 7 to 10 days. Sterile vascular access is needed.
•
Administered through the distal port of a central venous catheter. Reserve this port if you think initiating total parenteral nutrition (TPN) is a possibility—TPN cannot be given through a port that has already been used.
•
For initial orders and questions, a nutritional support consult will be valuable for information, advice, other options, and help with calculating projected nutritional needs.
•
TPN orders must be written daily and received by a certain time— make sure this is done before signing out.
•
Monitor vital signs, daily weight, I/Os, Accu-Cheks, and routine labs (CBC, electrolytes, BUN, Mg, phos) frequently. Monitor triglycerides and hepatic function at least once a week.
•
May add H2 blockers, steroids, insulin, and vitamin K to TPN if so desired.
•
If TPN must be stopped, monitor blood sugar and administer IV fluids (e.g., D10) at the same rate.
Guide to Procedures
23
VASCULAR ACCESS
Ultrasound-Guided Central Venous Access
•
The use of ultrasound guidance for the placement of central venous catheters is superior to the landmark-guided technique due to an improvement in average access time, reducing the number of attempts, and minimizing rates of complications.
•
Ultrasound guidance should be the method of choice for venous catheterization, especially in select populations (e.g., obese, critically ill, or history of multiple prior central venous catheters).
•
Indirect guidance
refers to assessing the vascular structures using 2D ultrasound prior to performing needle puncture and venous canalization.
•
Direct guidance
refers to the use of real-time ultrasound images during the needle puncture. The view can be either transverse (a cross section of the vein) or longitudinal (visualizing the vein on its long access). The transverse technique, which has been shown to be easier to learn by inexperienced physicians, will be described here.