Fundamentals of Midwifery: A Textbook for Students (153 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
6.43Mb size Format: txt, pdf, ePub
Apply pressure with tips of index and middle fingers to ANTERIOR shoulder to attempt to move shoulders into the oblique diameter. This is known as Rubin II manoeuvre.
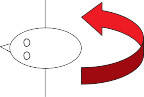 Anterior
Anterior
Posterior
 Anterior
AnteriorPosterior
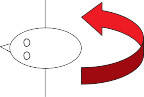
If no rotation occurs, use fingers of other hand to apply pressure to the anterior aspect of the POSTERIOR shoulder at the same time as applying pressure to the anterior shoulder as above. This is known as the Woodscrew manoeuvre.
 Anterior
Anterior
 366
366
Posterior
 Anterior
Anterior 366
366Posterior
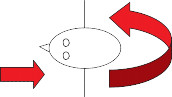
If there is still no rotation, remove second hand on anterior aspect of posterior shoulder and slide fingers of the first hand from the anterior shoulder to the posterior aspect of the POSTERIOR shoulder and attempt to rotate in the opposite direction. This is known as the reverse woodscrew manoeuvre.
 Anterior
Anterior
Posterior
Figure 16.8
Enter manoeuvres for shoulder dystocia.It is very important in these situations to allocate a member of the team to document the execution, timing and success of all manoeuvres employed to facilitate delivery. Documenting the position of the fetus, delivery time of the head, delivery time of the baby and head-to-body delivery interval is also an essential element of accurate record keeping.
NOTE: All enter manoeuvres should be completed within 60–90 seconds.
Thromboembolism
Thromboembolism is the term that encompasses the two pathological conditions of deep veinthrombosis (DVT) and pulmonary embolism (PE). Deep vein thrombosis is the formation of ablood clot (thrombus) in one of the deep veins, usually in the leg, resulting in partial or complete obstruction of the blood flow (National Institute for Health and Care Excellence (NICE) 2009). Pulmonary embolism is caused by a thrombus that has become dislodged and travelled back through the venous return and on to the vessels in the lung where it obstructs the pulmonary arterial system.Due to the effect of the physiological changes of pregnancy, the pregnant woman has a five times greater risk of developing these conditions (Springel 2013), especially if she develops some of the complications of pregnancy or has an operative delivery. Although these events can occur throughout the pregnancy, studies show that the highest incidence is during the first trimester and in the postpartum period where the risk has been estimated to be up to 20 times higher than in a non-pregnant woman of the same age (Greer 2012). As these conditions have serious implica- tions and prompt treatment is necessary, it is important for the midwife to understand when a woman may be at even greater risk from her medical history and require referral for consideration of thromboprophylaxis, as well as recognise the signs and symptoms of both conditions. (See Box 16.12 for the risk factors associated with venous thromboembolism.)Women in the high-risk group are recommended to have thromboprophylaxis through the pregnancy; those in the intermediate group should be considered for antenatal thrombo- prophylaxis; and those in the lower risk group should be advised regarding mobilisation and the avoidance of dehydration. This risk assessment should be undertaken at booking with the midwife, at any point during the pregnancy where the risk may be affected and in the postnatal period (see Chapter 8: ‘Postnatal midwifery care’ where thromboembolism is also discussed).
 367
367
 Box 16.12 Risk factors for venous thromboembolism (RCOG 2009)
Box 16.12 Risk factors for venous thromboembolism (RCOG 2009)
HIGH RISK
Known thrombophilia Previous recurrent VTE
INTERMEDIATE RISK
Previous history of VTE Family history of VTEMaternal disease: cardiac disease, systemic lupus erythematosus (SLE), Inflammatory bowel disease
OTHER FACTORS: 3 factors or more = INTERMEDIATE RISK; less than 3 = LOWER RISK
Obesity AnaemiaGross varicose veins SmokingSystemic infection Dehydration ImmobilityPre-eclampsia Multiple pregnancy Age >35
Signs and symptoms of a thromboembolism
Although a DVT does not always cause symptoms, the most common presentation is pain and/ or swelling in the lower leg; however many pregnant women have lower leg oedema making a clinical diagnosis difficult. Springel (2013) suggests a mid-calf circumference measurement of greater than 2 cm difference between the limbs may have more significance for DVT, especially if the problem is experienced in the left leg as the incidence of left DVT is higher in pregnancy.Similarly, many of the signs and symptoms of a PE are non-specific such as shortness of breath, cough and chest pain. Although these may be contributed to other causes, any suspi- cion of VTE must be treated whilst investigations are carried out to confirm or rule out the diagnosis (RCOG 2007).368
Management of a thromboembolism
Treatment for pregnant women with a DVT or PE is usually a twice daily regime of low molecular weight heparin (LMWH) such as Clexane or Fragmin, but the use of graduated compression stockings and leg elevation are also recommended (Greer 2012).
 In the case of sudden collapse of a pregnant woman, a massive PE should be suspected which is a life-threatening condition. Immediate resuscitative measures should be commenced as documented in the section on shock and basic life support. In the hospital setting an emergency call must be initiated. An urgent peri-mortem caesarean section may be required if the collapse occurs antenatally or during labour. In a community setting initial resuscitative measures should be undertaken after ensuring a 999 call is initiated first if alone.
In the case of sudden collapse of a pregnant woman, a massive PE should be suspected which is a life-threatening condition. Immediate resuscitative measures should be commenced as documented in the section on shock and basic life support. In the hospital setting an emergency call must be initiated. An urgent peri-mortem caesarean section may be required if the collapse occurs antenatally or during labour. In a community setting initial resuscitative measures should be undertaken after ensuring a 999 call is initiated first if alone.
 Key points
Key points
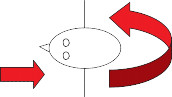
 Anterior
AnteriorPosterior
Figure 16.8
Enter manoeuvres for shoulder dystocia.It is very important in these situations to allocate a member of the team to document the execution, timing and success of all manoeuvres employed to facilitate delivery. Documenting the position of the fetus, delivery time of the head, delivery time of the baby and head-to-body delivery interval is also an essential element of accurate record keeping.
NOTE: All enter manoeuvres should be completed within 60–90 seconds.
Thromboembolism
Thromboembolism is the term that encompasses the two pathological conditions of deep veinthrombosis (DVT) and pulmonary embolism (PE). Deep vein thrombosis is the formation of ablood clot (thrombus) in one of the deep veins, usually in the leg, resulting in partial or complete obstruction of the blood flow (National Institute for Health and Care Excellence (NICE) 2009). Pulmonary embolism is caused by a thrombus that has become dislodged and travelled back through the venous return and on to the vessels in the lung where it obstructs the pulmonary arterial system.Due to the effect of the physiological changes of pregnancy, the pregnant woman has a five times greater risk of developing these conditions (Springel 2013), especially if she develops some of the complications of pregnancy or has an operative delivery. Although these events can occur throughout the pregnancy, studies show that the highest incidence is during the first trimester and in the postpartum period where the risk has been estimated to be up to 20 times higher than in a non-pregnant woman of the same age (Greer 2012). As these conditions have serious implica- tions and prompt treatment is necessary, it is important for the midwife to understand when a woman may be at even greater risk from her medical history and require referral for consideration of thromboprophylaxis, as well as recognise the signs and symptoms of both conditions. (See Box 16.12 for the risk factors associated with venous thromboembolism.)Women in the high-risk group are recommended to have thromboprophylaxis through the pregnancy; those in the intermediate group should be considered for antenatal thrombo- prophylaxis; and those in the lower risk group should be advised regarding mobilisation and the avoidance of dehydration. This risk assessment should be undertaken at booking with the midwife, at any point during the pregnancy where the risk may be affected and in the postnatal period (see Chapter 8: ‘Postnatal midwifery care’ where thromboembolism is also discussed).
 367
367 Box 16.12 Risk factors for venous thromboembolism (RCOG 2009)
Box 16.12 Risk factors for venous thromboembolism (RCOG 2009)HIGH RISK
Known thrombophilia Previous recurrent VTE
INTERMEDIATE RISK
Previous history of VTE Family history of VTEMaternal disease: cardiac disease, systemic lupus erythematosus (SLE), Inflammatory bowel disease
OTHER FACTORS: 3 factors or more = INTERMEDIATE RISK; less than 3 = LOWER RISK
Obesity AnaemiaGross varicose veins SmokingSystemic infection Dehydration ImmobilityPre-eclampsia Multiple pregnancy Age >35
Signs and symptoms of a thromboembolism
Although a DVT does not always cause symptoms, the most common presentation is pain and/ or swelling in the lower leg; however many pregnant women have lower leg oedema making a clinical diagnosis difficult. Springel (2013) suggests a mid-calf circumference measurement of greater than 2 cm difference between the limbs may have more significance for DVT, especially if the problem is experienced in the left leg as the incidence of left DVT is higher in pregnancy.Similarly, many of the signs and symptoms of a PE are non-specific such as shortness of breath, cough and chest pain. Although these may be contributed to other causes, any suspi- cion of VTE must be treated whilst investigations are carried out to confirm or rule out the diagnosis (RCOG 2007).368
Management of a thromboembolism
Treatment for pregnant women with a DVT or PE is usually a twice daily regime of low molecular weight heparin (LMWH) such as Clexane or Fragmin, but the use of graduated compression stockings and leg elevation are also recommended (Greer 2012).
 In the case of sudden collapse of a pregnant woman, a massive PE should be suspected which is a life-threatening condition. Immediate resuscitative measures should be commenced as documented in the section on shock and basic life support. In the hospital setting an emergency call must be initiated. An urgent peri-mortem caesarean section may be required if the collapse occurs antenatally or during labour. In a community setting initial resuscitative measures should be undertaken after ensuring a 999 call is initiated first if alone.
In the case of sudden collapse of a pregnant woman, a massive PE should be suspected which is a life-threatening condition. Immediate resuscitative measures should be commenced as documented in the section on shock and basic life support. In the hospital setting an emergency call must be initiated. An urgent peri-mortem caesarean section may be required if the collapse occurs antenatally or during labour. In a community setting initial resuscitative measures should be undertaken after ensuring a 999 call is initiated first if alone. Key points
Key pointsRecognition and response to emergencies by midwives can make a significant difference to the
 outcome for women and their families.
outcome for women and their families.

 outcome for women and their families.
outcome for women and their families.
Other books
Shadowbred by Kemp, Paul S.
The Faery Princess by Marteeka Karland
The Confidence Code by Katty Kay, Claire Shipman
The Outlaw Takes a Bride by Susan Page Davis
Strength of Stones by Greg Bear
The Gandhian Adventures of Raj & Iqbal: A Novel by Zubin J. Shroff
THE CINDER PATH by Yelena Kopylova
Sweet on You by Kate Perry
Loose Cannon by Sharon Lee and Steve Miller, Steve Miller
Diary Of A Pissed Off Wife by Jordan Silver