Fundamentals of Midwifery: A Textbook for Students (84 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
6.94Mb size Format: txt, pdf, ePub
2
O and to enable the fluid to be pushed back into the circulating volume this needs to be maintained for two to three seconds. This should be repeated for five inflations and then reassessment can take place. It is important to watch for chest movement during this procedure to confirm air entry, but the more certain indicator of successful lung inflation is an increase in the heart rate. Once lung inflation has been achieved many babies will begin regular respira- tions, but if not further assistance will be required with ventilation or they will once again become hypoxic and bradycardic. The same technique is used but these ventilation breaths are at a rate of 30 per minute so are a shorter duration of only one second with one second gaps. If regular respiration still does not occur, then further intervention may be required and per- sonnel with further training may need to take over the resuscitation, but efficient use of these basic methods will maintain the airway until appropriate staff is available. It is important to inform any personnel involved if the mother has received opiates during her labour as this may have a respiratory depressant effect on the baby. Other information that may indicate an increased risk of infection or respiratory problems such as prolonged rupture of membranes or meconium stained liquor must also be passed on to any incoming personnel (see Figure 9.3,which illustrates the basic care and resuscitation algorithm for the newborn).
Immediate care of the newborn
For the majority of babies who do not require resuscitation, the immediate transition into extra-uterine life can be accomplished in a more natural way. The NICE Guideline for Intrapartum Care (Hutton and Hassan 2007) suggests that if the Apgar score at one minute is five or less then the cord should be double clamped to enable the collection of paired cord samples to analyse cord gases; however in other cases early cord clamping is not recommended. Very early cord clamp- ing has been suggested to contribute to hypovolaemia and anaemia and a delay in cord clamp- ing of at least two minutes has been shown in a review of controlled trials to improve the haematological and iron status of the term infant in both the short and long term, up to six months of age (Hutton and Hassan 2007). The concerns of a higher haematocrit and increased jaundice due to the placental transfusion resulting from delayed clamping were not found to have any clinical significance even when active management of the third stage is undertaken. The Resuscitation Council UK (2010) recommend for uncompromised babies, a delay in cord clamping of at least one minute from the complete delivery of the infant.A further important contributor towards this transition is the use of skin-to-skin contact with the mother. which involves placing the naked infant prone on the mother’s chest. Studies have found numerous benefits of skin-to-skin contact immediately after birth for mother and baby including stabilisation of the cardiovascular system, better thermoregulation, higher blood glucose levels, earlier initiation of breastfeeding, and a reduction in crying and improved breast- feeding rates up to four months of age (Moore et al. 2012). It is important to note that this same review highlighted some factors that may impact on the effectiveness of skin-to-skin care such as room temperature, modesty and lack of privacy. Therefore the midwife should endeavour to create an environment conducive to this practice whilst respecting the fact that the decision to do so is ultimately the mother’s choice. If undertaken, it is important to ensure a few simple measures are utilised. The infant will need to be dried and a cover placed over mother and baby as heat loss will occur via wet skin due to evaporation and from cooler air draughts through convection. To prevent heat loss via conduction and radiation, the contact with the mother
 193
193
Dry the baby
This should be the first action in all cases except where meconium liquor was present or prematurity indicates wrapping
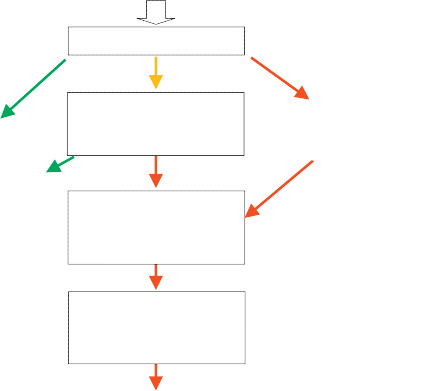 Assess first Apgar score
Assess first Apgar score
 194If infant is pale, floppy and bradycardic
194If infant is pale, floppy and bradycardic
Call for help
if appropriate personnel not present.If infant has good tone and a heart rate of below 100bpm allow a little more time for respirations to establish up to 90 seconds in totalIf Apgar score
above 7
baby can be given to mother for SKIN TO SKIN CARE if sheconsents.
Maintain airway
by placing in a neutral position. A jaw thrust manoeuvre or the insertion of an airway may be necessary if the tongue is obstructing the airway.If infant is not breathing despite airway opening manoeuvres give
5 Inflation breaths
via facemask at 30 cm H
2
O pressure with air initially.
Re-assess
and continue ventilation breaths at a lower pressure if necessary.
Figure 9.3
Basic care and resuscitation of the newborn.should be directly on the skin and not through clothing or bed covers. The head will need to be covered with either a cover or hat as this area loses the most heat. (See Table 9.3 for more information regarding heat loss mechanisms.) Necessary procedures such as weighing the baby (see Figure 9.5) should ideally occur prior to commencement of skin-to-skin or very soon after- wards with the infant being returned to mother directly, to enable the early initiation of breast- feeding where appropriate; other procedures such as measurements and initial examination may be performed whilst allowing skin-to-skin contact to continue.An initial examination of the newborn infant for any obvious abnormalities should be carried out by the midwife following birth. This should include a head to toe check done with the parents’ consent and ideally in their presence (NICE 2006). A more comprehensive examination will be carried out prior to discharge, but this initial examination remains vital in the early
Table 9.2
Examining the newborn infant
 Head
Head
Moulding (overriding of the bones of the skull) and caput succedaneum (oedema of the scalp) are common but generally resolve within 48 hours. Parents will often need reassurance that their baby’s misshapen head is not a sign of abnormality. However excessive moulding or cephalhaematoma (bleeding between the periosteum and the bone) should be noted and the baby observed for any signs of cerebral birth trauma.
Face
Abnormal facial appearance may indicate conditions such as palsy or syndromes (e.g. Edward’s) but it is sensible to see both parents before placing too much weight on appearance alone. Any marks from instrumental delivery should be explained to parents.
Eyes
Always check that both eyes are present as this cannot be ascertained when the eyelids are closed.
Ears
The position of the ears should be noted as low set ears are associated with some syndromes.
Mouth
Checking that the palate is properly formed without a cleft is important. Inserting a clean to feel the palate is a common method of choice or inspect with a light which may reveal a sub-mucus cleft. Visualisation is essential to ensure smaller clefts are not missed. Inspection of the mouth also gives the midwife some idea of the sucking reflex (see Figure 9.4).
Genitalia
Check for any obvious abnormality.
Anus
Check for position and apparent patency.
Back
Run a finger down the spine to check for any indentations or swellings. Some babies may have an area of blue discolouration around the sacrum and buttock area; this is particularly common in some racial groups and is normal.
Limbs
Check fingers and toes for missing or extra digits and for any webbing.195recognition of gross abnormality and also in beginning the process of parent education in the care of their new infant.In addition to examining the baby as detailed in Table 9.2, the baby should be weighed and measurements of head circumference (occipito-frontal circumference) and length should be taken. These measurements should be considered against ‘norms’ for gestational age, but it should be remembered that moulding may affect head circumference. It is generally accepted practice to gain consent for administration of vitamin K at this time (NICE 2006). Vitamin K is essential for effective blood clotting and is given to prevent rare but life-threatening haemor- rhagic disease of the newborn. It is ideally given as an intramuscular injection (1 mg) but if parents are unwilling to consent to this method of administration NICE guidance (NICE 2006) suggests offering oral treatment as an option (see Chapter 15: ‘Pharmacology and medicines management’ and refer to the monographs where vitamin K is discussed in more depth). If parents decline vitamin K, they should be provided with advice about symptoms that would indicate possible vitamin K deficiency bleeding. These symptoms include: bleeding, bruising or petichiae unrelated to any known trauma and symptoms associated with intracranial bleeding (irritability, high pitched crying, pallor, loss of appetite, vomiting).
Maintaining health in the first few days of life
It is essential in the first few days of life that the infant is kept warm and that feeding is established.Any deviations from the normal should be recognised quickly and appropriate action taken. The care provided should be aimed at keeping the baby PINK, WARM AND SWEET. This is because196


O and to enable the fluid to be pushed back into the circulating volume this needs to be maintained for two to three seconds. This should be repeated for five inflations and then reassessment can take place. It is important to watch for chest movement during this procedure to confirm air entry, but the more certain indicator of successful lung inflation is an increase in the heart rate. Once lung inflation has been achieved many babies will begin regular respira- tions, but if not further assistance will be required with ventilation or they will once again become hypoxic and bradycardic. The same technique is used but these ventilation breaths are at a rate of 30 per minute so are a shorter duration of only one second with one second gaps. If regular respiration still does not occur, then further intervention may be required and per- sonnel with further training may need to take over the resuscitation, but efficient use of these basic methods will maintain the airway until appropriate staff is available. It is important to inform any personnel involved if the mother has received opiates during her labour as this may have a respiratory depressant effect on the baby. Other information that may indicate an increased risk of infection or respiratory problems such as prolonged rupture of membranes or meconium stained liquor must also be passed on to any incoming personnel (see Figure 9.3,which illustrates the basic care and resuscitation algorithm for the newborn).
Immediate care of the newborn
For the majority of babies who do not require resuscitation, the immediate transition into extra-uterine life can be accomplished in a more natural way. The NICE Guideline for Intrapartum Care (Hutton and Hassan 2007) suggests that if the Apgar score at one minute is five or less then the cord should be double clamped to enable the collection of paired cord samples to analyse cord gases; however in other cases early cord clamping is not recommended. Very early cord clamp- ing has been suggested to contribute to hypovolaemia and anaemia and a delay in cord clamp- ing of at least two minutes has been shown in a review of controlled trials to improve the haematological and iron status of the term infant in both the short and long term, up to six months of age (Hutton and Hassan 2007). The concerns of a higher haematocrit and increased jaundice due to the placental transfusion resulting from delayed clamping were not found to have any clinical significance even when active management of the third stage is undertaken. The Resuscitation Council UK (2010) recommend for uncompromised babies, a delay in cord clamping of at least one minute from the complete delivery of the infant.A further important contributor towards this transition is the use of skin-to-skin contact with the mother. which involves placing the naked infant prone on the mother’s chest. Studies have found numerous benefits of skin-to-skin contact immediately after birth for mother and baby including stabilisation of the cardiovascular system, better thermoregulation, higher blood glucose levels, earlier initiation of breastfeeding, and a reduction in crying and improved breast- feeding rates up to four months of age (Moore et al. 2012). It is important to note that this same review highlighted some factors that may impact on the effectiveness of skin-to-skin care such as room temperature, modesty and lack of privacy. Therefore the midwife should endeavour to create an environment conducive to this practice whilst respecting the fact that the decision to do so is ultimately the mother’s choice. If undertaken, it is important to ensure a few simple measures are utilised. The infant will need to be dried and a cover placed over mother and baby as heat loss will occur via wet skin due to evaporation and from cooler air draughts through convection. To prevent heat loss via conduction and radiation, the contact with the mother
 193
193Dry the baby
This should be the first action in all cases except where meconium liquor was present or prematurity indicates wrapping
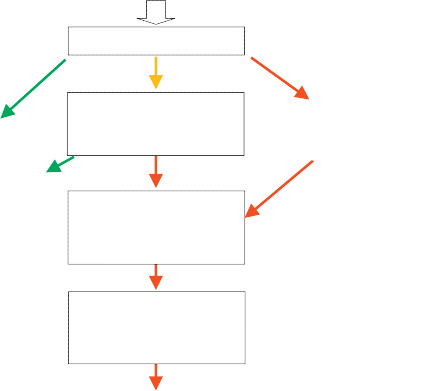 Assess first Apgar score
Assess first Apgar score 194If infant is pale, floppy and bradycardic
194If infant is pale, floppy and bradycardicCall for help
if appropriate personnel not present.If infant has good tone and a heart rate of below 100bpm allow a little more time for respirations to establish up to 90 seconds in totalIf Apgar score
above 7
baby can be given to mother for SKIN TO SKIN CARE if sheconsents.
Maintain airway
by placing in a neutral position. A jaw thrust manoeuvre or the insertion of an airway may be necessary if the tongue is obstructing the airway.If infant is not breathing despite airway opening manoeuvres give
5 Inflation breaths
via facemask at 30 cm H
2
O pressure with air initially.
Re-assess
and continue ventilation breaths at a lower pressure if necessary.
Figure 9.3
Basic care and resuscitation of the newborn.should be directly on the skin and not through clothing or bed covers. The head will need to be covered with either a cover or hat as this area loses the most heat. (See Table 9.3 for more information regarding heat loss mechanisms.) Necessary procedures such as weighing the baby (see Figure 9.5) should ideally occur prior to commencement of skin-to-skin or very soon after- wards with the infant being returned to mother directly, to enable the early initiation of breast- feeding where appropriate; other procedures such as measurements and initial examination may be performed whilst allowing skin-to-skin contact to continue.An initial examination of the newborn infant for any obvious abnormalities should be carried out by the midwife following birth. This should include a head to toe check done with the parents’ consent and ideally in their presence (NICE 2006). A more comprehensive examination will be carried out prior to discharge, but this initial examination remains vital in the early
Table 9.2
Examining the newborn infant
 Head
HeadMoulding (overriding of the bones of the skull) and caput succedaneum (oedema of the scalp) are common but generally resolve within 48 hours. Parents will often need reassurance that their baby’s misshapen head is not a sign of abnormality. However excessive moulding or cephalhaematoma (bleeding between the periosteum and the bone) should be noted and the baby observed for any signs of cerebral birth trauma.
Face
Abnormal facial appearance may indicate conditions such as palsy or syndromes (e.g. Edward’s) but it is sensible to see both parents before placing too much weight on appearance alone. Any marks from instrumental delivery should be explained to parents.
Eyes
Always check that both eyes are present as this cannot be ascertained when the eyelids are closed.
Ears
The position of the ears should be noted as low set ears are associated with some syndromes.
Mouth
Checking that the palate is properly formed without a cleft is important. Inserting a clean to feel the palate is a common method of choice or inspect with a light which may reveal a sub-mucus cleft. Visualisation is essential to ensure smaller clefts are not missed. Inspection of the mouth also gives the midwife some idea of the sucking reflex (see Figure 9.4).
Genitalia
Check for any obvious abnormality.
Anus
Check for position and apparent patency.
Back
Run a finger down the spine to check for any indentations or swellings. Some babies may have an area of blue discolouration around the sacrum and buttock area; this is particularly common in some racial groups and is normal.
Limbs
Check fingers and toes for missing or extra digits and for any webbing.195recognition of gross abnormality and also in beginning the process of parent education in the care of their new infant.In addition to examining the baby as detailed in Table 9.2, the baby should be weighed and measurements of head circumference (occipito-frontal circumference) and length should be taken. These measurements should be considered against ‘norms’ for gestational age, but it should be remembered that moulding may affect head circumference. It is generally accepted practice to gain consent for administration of vitamin K at this time (NICE 2006). Vitamin K is essential for effective blood clotting and is given to prevent rare but life-threatening haemor- rhagic disease of the newborn. It is ideally given as an intramuscular injection (1 mg) but if parents are unwilling to consent to this method of administration NICE guidance (NICE 2006) suggests offering oral treatment as an option (see Chapter 15: ‘Pharmacology and medicines management’ and refer to the monographs where vitamin K is discussed in more depth). If parents decline vitamin K, they should be provided with advice about symptoms that would indicate possible vitamin K deficiency bleeding. These symptoms include: bleeding, bruising or petichiae unrelated to any known trauma and symptoms associated with intracranial bleeding (irritability, high pitched crying, pallor, loss of appetite, vomiting).
Maintaining health in the first few days of life
It is essential in the first few days of life that the infant is kept warm and that feeding is established.Any deviations from the normal should be recognised quickly and appropriate action taken. The care provided should be aimed at keeping the baby PINK, WARM AND SWEET. This is because196


Other books
Scam on the Cam by Clémentine Beauvais
Zooey Pinkerton- a Daughter's Right by Heather McAlendin
Linebacker's Second Chance (Bad Boy Ballers) by Imani King
INK: Red (INK Trilogy Book 1) by Line, Al K.
Cabin Fever: The sizzling secrets of a Virgin air hostess… by Mandy Smith
El alfabeto de Babel by Francisco J de Lys
The Wolfe Widow (A Book Collector Mystery) by Victoria Abbott
Dragon's Egg by Robert L. Forward
Rip Tides by Toby Neal