Read Pediatric Primary Care Case Studies Online
Authors: Catherine E. Burns,Beth Richardson,Cpnp Rn Dns Beth Richardson,Margaret Brady
Tags: #Medical, #Health Care Delivery, #Nursing, #Pediatric & Neonatal, #Pediatrics
Pediatric Primary Care Case Studies (18 page)

BOOK: Pediatric Primary Care Case Studies
4.15Mb size Format: txt, pdf, ePub
ads
• Family history of diseases
Functional health patterns:
• Nutrition: Appetite and 24-hour diet recall (note type and frequency of carbohydrate intake, caloric restrictions, caffeine use)
• Sleep and rest: Thorough sleep history including normal sleep habits and the presence of insomnia or parasomnias
• Psychosocial history
Job history and occupational exposures (note numbers of hours worked, time of day worked, and chemical/infectious exposures)
Family life issues
School issues
Developmental history:
• Independence from parents
• Peer relationships
• Sexual patterns
• Vocational issues
• Cognitive level
Jennifer reveals that she has had no recent travel except for a weekend trip to the beach with her family. She denies fever and is able to keep up her daily routines despite
her fatigue. There is no history of recent tick, mosquito, or other insect bites. No one at home is ill, and she has no known sick contacts. She denies feelings of sadness, impaired concentration, and alcohol, tobacco, or other substance use. Jennifer’s mom has hypothyroidism and takes “some pill once a day” to treat it.
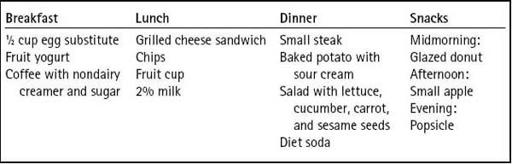
Routine medications include daily use of a multivitamin with iron and ibuprofen 600 mg every 6 hours as needed for menstrual discomfort. She has seasonal allergies but is not currently taking medication for them. Jennifer reports that she is not currently sexually active and that she is currently menstruating so her last dose of ibuprofen was this morning. Her 24-hour diet recall is listed in
Table 5-1
. Jennifer states that she keeps a water bottle with her at work and she drinks at least 36 ounces of water a day. She denies constipation and diarrhea. She has no polyuria or dysuria.
Jennifer has an active social life and tries to get together with her friends “at least two to three times a week” but she has been “hanging out” with her closest circle of friends “most nights since summer is almost over.” Hanging out usually consists of meeting at a friend’s house, watching TV or playing video games, and listening to music. She is a senior in high school and achieves A and B grades without difficulty and anticipates going to college next year, though without a vocation in mind.
Jennifer has two jobs over the summer. She works 4 days a week at the local swimming pool. Her workday typically begins at 10 a.m. and ends around 6:30 p.m. Three days during the work week and one day on the weekend she babysits her neighbor’s two children in the evening. During the week, she goes from the pool directly to her neighbor’s and works until 10 p.m. On Saturday, she babysits from 7:30 a.m. until 4 p.m. She is allowed to sleep after the children go to sleep, but she is usually awake when the mother comes home because “their sofa is too uncomfortable to sleep on and I am usually chatting with my friends online.” Most evenings, Jennifer falls asleep around midnight, “but there are nights I watch movies until 2 a.m.” She sets her alarm to wake her at 7:30 a.m. but admits she often uses the snooze button three to four times before getting up. Jennifer falls asleep listening to her MP3 player, and she reports often awakening 2 to 3 hours after falling asleep to find her lights are on and her music is still playing.
Given these history findings, what is the most likely cause of Jennifer’s fatigue?
Table 5–1 Jennifer’s 24-Hour Diet Recall
What additional questions regarding Jennifer’s sleep habits would help establish the diagnosis?
Physical Examination Findings
Jennifer is a well-groomed adolescent with a normal affect. Her mental status is normal. Her height is 5′6″, and her weight is 145 pounds (BMI 23.4). There are no rashes or lymphadenopathy and her vital signs are normal. Skin tone is nonjaundiced and capillary refill is less than 2 seconds in all extremities. There is no nasal turbinate edema, her conjunctiva are noninjected, and her tympanic membranes and oropharynx are normal. Jennifer’s thyroid is nontender, normal sized, and without palpable lesions. There are no heart murmurs, and her heart rate is regular. Lung sounds are clear, and there are no signs of allergy, cyanosis, or clubbing. Both liver and spleen are nonpalpable, and the other abdominal exam findings are negative. Neurologic exam reveals 2+ deep tendon reflexes (DTRs) in all extremities with normal movement, strength, and sensation. All other exam findings are normal. Pelvic examination is deferred.
Is it possible Jennifer’s fatigue is caused by a significant medical condition?
What diagnostic testing can be used to determine the cause of Jennifer’s fatigue?
While performing the physical examination, Jennifer’s cell phone rings, and her mother asks to speak with you. The mother requests that you test Jennifer for mononucleosis and hypothyroidism because she first showed symptoms of hypothyroidism during her junior year of high school. You talk to Jennifer about her mother’s request, and Jennifer agrees to the testing. Laboratory findings are as follows:
Complete blood count (CBC): WBC 6.2 × 10
3
/mm
3
(normal), RBC 4.7 million/mL (normal), hematocrit 40% (normal), and hemoglobin 13.2 g/dL (normal).

BOOK: Pediatric Primary Care Case Studies
4.15Mb size Format: txt, pdf, ePub
ads
Other books
Her Favorite Rival by Sarah Mayberry
Fixer by Gene Doucette
Visa Run - Pattaya to Sihanoukville by Peter Jaggs
The Sweetest Thing by J. Minter
Without You, There Is No Us by Suki Kim
Blissful volume 3 (New Adult Romance) by Wild, Clarissa
Steel: (#5 The Beat and the Pulse) by Amity Cross
Undefeated: Bad Boy Fighter Romance (Fighting For Gisele #4) by Emily Jane Trent
Klepto by Jenny Pollack
Falafel Jones - Max Fried 02 - Payback's a Beach by Falafel Jones
