Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (113 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

angiogram
(mesenteric or renal vessels) →
microaneurysms
& focal vessel narrowing
CTA may be adequate to make dx, but conventional angiogram is most sensitive
biopsy
(sural nerve, skin or affected organ) → vasculitis of small and medium vessel arteries with fibrinoid necrosis without granulomas
• Treatment:
steroids
± CYC (if severe or failure to induce remission); antivirals if a/w HBV
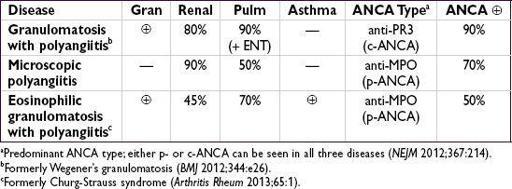
ANCA-ASSOCIATED SMALL-VESSEL VASCULITIS
Microvascular vasculitis (eg, capillaries, postcapillary venules, & arterioles)
Differential diagnosis of ANCA
•
anti-PR3 (c-ANCA)
: granulomatosis w/ polyangiitis, eosinophilic granulomatosis and polyangiitis, microscopic polyangiitis (rarely) •
anti-MPO (p-ANCA)
: microscopic polyangiitis, eosinophilic granulomatosis and
polyangiitis, granulomatosis w/ polyangiitis, drug-induced vasculitis, nonvasculitic
rheumatic diseases
•
Atypical ANCA patterns
: drug-induced vasculitis, nonvasculitic rheumatic diseases,
ulcerative colitis, primary sclerosing cholangitis, endocarditis, cystic fibrosis
Granulomatosis with polyangiitis
(GPA, formerly Wegener’s granulomatosis)
•
Necrotizing granulomatous systemic vasculitis
frequently affecting nose, sinuses and/or upper respiratory tract in addition to kidneys, lungs,
etc.
• Epidemiology: any age, but ↑ incidence in young and middle-aged adults;=
• Clinical manifestations
respiratory
(90%)
upper
: sinusitis, rhinitis, oral/nasal ulcers, saddle-nose deformity, otitis, hearing loss, subglottic stenosis
lower
: pulmonary infiltrates, nodules, pulmonary hemorrhage, hemoptysis, pleurisy
renal
(80%):
RPGN
(pauci-immune), RBC casts, dysmorphic RBCs, hematuria
ocular (50%): episcleritis, scleritis, uveitis, orbital granulomas → proptosis, corneal ulcer
neurologic: cranial and peripheral neuropathies, mononeuritis multiplex
skin (50%): palpable purpura, livedo reticularis
hematologic: ↑ incidence DVT/PE (20×) when disease active (Ann Intern Med 2005;142:620)
• Dx studies:
90%ANCA
(80% PR3, 20% MPO), less Se in limited upper airway disease
CXR or CT → nodules, infiltrates, cavities; sinus CT → sinusitis ± bone erosions
↑ BUN & Cr, proteinuria, hematuria; sediment w/ RBC casts, dysmorphic RBCs
Biopsy → necrotizing granulomatous inflammation of arterioles, capillaries, veins
• Treatment (Annals 2009;150:670; NEJM 2010;363:211 & 221)
Induction:
RTX
(375 mg/m
2
/wk × 4 wk) +
steroids
(1 g IV × 3 Δ → 1–2 mg/kg/d) or
CYC
(2 mg/kg/d × 3–6 mo or pulse 15 mg/kg q2–3wk) + steroids
RPGN: ± plasma exchange to ? ↓ risk of ESRD (Am J Kidney Dis 2011;57:566)
if mild (nonorgan-or life-threatening): MTX + prednisone
may
be adequate for induction (Arth Rheum 2012;64:3472)
Maintenance
:
MTX
or
AZA
for ≥2 y after CYC induction (NEJM 2008;359:2790); after RTX induction repeat RTX q6mo (Arth Rheum 2012;64:3760) vs. watchful waiting
Relapse
: if severe, reinduce w/ steroids + RTX or CYC; steroids ± MTX or AZA if mild;
↑ ANCA w/o clinical evidence of flare should not prompt Δ Rx (Annals 2007;147:611)
Microscopic polyangiitis (MPA)
(
Rheum Dis Clin North Am
2010;36:545)
• Similar to GPA, but
w/o ENT/airway involvement & nongranulomatous
• Epidemiology: >
> ; avg onset 50–60 y • Clinical manifestations: similar to GPA w/o upper respiratory involvement;
; avg onset 50–60 y • Clinical manifestations: similar to GPA w/o upper respiratory involvement;
renal
(80–100%): glomerulonephritis
pulmonary
(25–50%): pulmonary capillary alveolitis, pulmonary fibrosis constitutional and neuro sx similar to GPA; skin lesions (eg, palpable purpura) in 30–60%
• Dx studies:
70%ANCA
(almost all anti-MPO)
biopsy → necrotizing,
nongranulomatous
inflammation of small vessels, pauci-immune (minimal deposition of complement or Ig; contrast w/ HSP, cryoglobulinemia, etc.)
urine sediment and CXR findings similar to those seen in GPA
• Treatment: as for GPA; ↓ relapse rate compared to GPA
Eosinophilic granulomatosis with polyangiitis
(EGPA, formerly Churg-Strauss)
• Similar to GPA w/ more frequent
cardiac involvement
, a/w
asthma
and
eosinophilia
• Epidemiology: rare; can present at any age (typically 30–40 y); a/w HLA-DRB4
• Clinical manifestations (Curr Rheumatol Rep 2011;13:489)
initial sx:
asthma
, sinusitis, allergic rhinitis (new asthma in adult raises suspicion)
eosinophilic infiltrative disease: shifting or transient
pulmonary infiltrates
, gastroenteritis or esophagitis
systemic small-vessel vasculitis:
neuropathy
(mononeuritis multiplex), renal (glomerulonephritis), skin (palpable purpura, petechial, nodules)
cardiac
: coronary arteritis, myocarditis, CHF, valvular insufficiency (Medicine 2009;88:236)
• Dx studies: 50%ANCA (MPO > PR3),
eosinophilia
(5–10 k/µL, 80–100%),