Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (117 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
4.03Mb size Format: txt, pdf, ePub
• Treat any underlying causes, including CNS infections, intoxication, withdrawal,
etc.
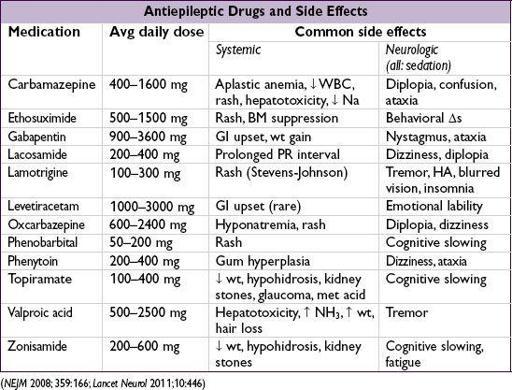
• Antiepileptic drug (AED) therapy is usually reserved for Pts w/ underlying structural abnormality or an idiopathic seizure
plus
(i) status epilepticus on presentation, (ii) focal neurologic exam, (iii) postictal Todd’s paralysis or (iv) abnormal EEG
• After 1st unprovoked sz, if EEG and MRI nl → 65% sz-free at 5 y (
Lancet Neurol
2006;5:317) • For Pts w/ infrequent seizures, early (vs. delayed) intervention w/ AED ↑ time to seizure recurrence, but has no effect on long-term seizure-free status (
Lancet
2005;365:2007) • AED choice dependent on type of seizure, side effects, cost, mechanism of elimination (if hepatic or renal insufficiency), teratogenesis and drug interactions • Introduce gradually, monitor carefully • May consider withdrawal if seizure-free (typically for at least 1 y) and normal EEG
• Individual state laws mandate seizure-free duration before being allowed to drive
Status epilepticus (consult neurology)
• Place Pt in semiprone position to ↓ risk of aspiration • Oral airway or, if prolonged, endotracheal intubation • IV access, start normal saline infusion • STAT labs including glc, Na, Ca, serum & urine toxicology screen, anticonvulsant levels • Thiamine (100 mg IV)
prior to d
extrose to prevent Wernicke’s encephalopathy • Dextrose (50 g IV push)
ALCOHOL WITHDRAWAL
Pathophysiology
• Alcohol is a CNS depressant • Chronic use → insensitivity to inhibitory neurotransmitter g-aminobutyric acid (GABA) • Abrupt alcohol cessation → CNS overactivity
Clinical manifestations
• Minor withdrawal sx (6–48 h after last drink): mild anxiety, tremulousness, HA •
Withdrawal seizures
: typically w/in 48 h after last drink; if unRx’d,
1
⁄
3
→ delirium tremens •
Alcoholic hallucinosis
: isolated hallucinations (typically visual) 12–48 h after last drink •
Delirium tremens
(
DT
): disorientation, agitation, hallucinations, ↑ HR & BP, fever, diaphoresis; begins 48–96 h after last drink, lasts 5–7 d • Consider other dx: CNS infxn or bleed, sz, drug O/D, coingestions, acute liver failure, GIB
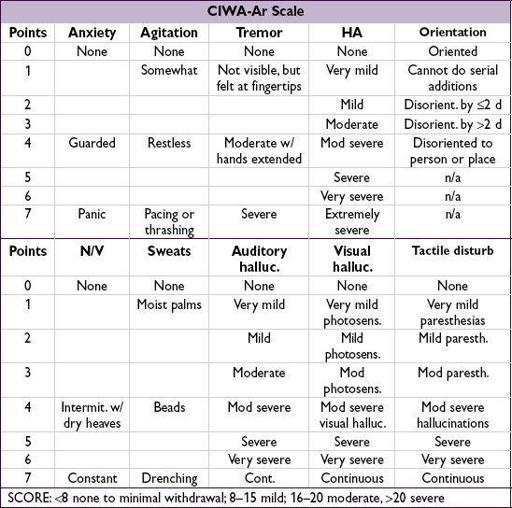
Clinical Institute Withdrawal Assessment scale for alcohol (CIWA-Ar)
• Assign points for each of the 10 criteria; each criteria is scored 0–7 except orientation which is scored 0–4; add points to calculate score
Treatment (
NEJM
2003;348:1786)
•
Benzodiazepines
(BDZ)
Drug: diazepam (long-acting w/ active metab; ↓ risk of recurrent withdrawal), lorazepam (short half-life), chlordiazepoxide, oxazepam (no active metab; good if cirrhosis)
Route: start IV, transition to PO
Dosing: typically start w/ diazepam 10–15 mg IV q10–15min (or lorazepam 2–4 mg IV q15–20min) until appropriate sedation achieved, then titrate to CIWA-Ar scale, evaluating q1h until score <8 × 8 h, then q2h × 8 h, and if stable, then q4h (
JAMA
1994;272:519)
• If refractory to BDZ prn, consider BDZ gtt, phenobarbital or propofol (& intubation) •
Avoid
haloperidol (↓ seizure threshold) or βB/central ɑ
2
-agonists (mask sx) • Mechanical restraints as needed until chemical sedation achieved • Volume resuscitation as needed; thiamine
then
glc to prevent
Wernicke’s encephalopathy
(ataxia, ophthalmoplegia, short-term memory loss); replete K, Mg, PO
4
• Prophylaxis: if min sx or asx (ie, CIWA score <8) but prolonged heavy EtOH con-sumption or h/o withdrawal seizures or DTs → chlordiazepoxide 25–100 mg (based on severity of EtOH use) q6h × 24 h, then 25–50 mg q6h × 2 d
STROKE
ISCHEMIC STROKE
Etiologies
• Embolic (~75%): artery → artery, cardioembolic, paradoxical (
NEJM
2007;357:2262), cryptogenic • Thrombotic (~25%): large vessel (atherosclerosis) vs. small vessel (“lacunar,” lipohyalinosis of small arteries, often related to HTN, hyperlipidemia, & DM) • Other: dissection, vasculitis, vasospasm, prothrombotic states, hypoperfusion, genetic
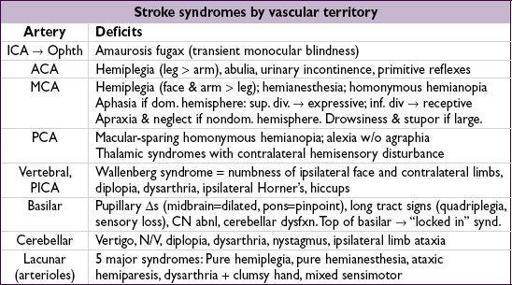
Clinical Manifestations
• Timing: embolic → sudden onset; thrombotic → stuttering course
Transient ischemic attack (TIA)
• Sudden deficit due to cerebral ischemia;
no stroke on imaging
; sx resolve <24 h (most <1 h) • Ddx: seizure, migraine, hypoglycemia, amyloid spells, TGA, anxiety • Risk of subsequent stroke per
ABCD
2
:
A
ge ≥60 y (+1);
B
P ≥140/90 (+1);
C
lin features: unilat. weak. (+2), speech impair. w/o weakness (+1);
D
uration ≥60 (+2) or 10–59 min (+1);
D
M (+1)
risk of stroke at 48 h: low risk (0–3) = 1.0%; moderate (4–5) = 4.1%; high (6–7) = 8.1%
Physical exam
• General: assess for arrhythmias, murmurs, carotid & subclavian bruits, peripheral emboli • Neurologic exam, NIH stroke scale (
http://www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf
)
Acute workup (w/in 8 h for anterior and w/in 24 h for posterior circulation)
• Electrolytes, Cr (relevant for contrast); glc, CBC, coags (see exclusion criteria for lysis) • Cardiac biomarkers, 12-lead ECG, tox screen •
STAT CT
to r/o ICH prior to lysis (SeMRI, faster, more widely available)
early signs: hyperdense artery, loss of gray-white differentiation, edema, insular ribbon
CT can be nl in first hrs after sx onset, not Se for small strokes & brainstem strokes
obtain CT-angio head & neck or CT perfusion if endovascular intervention indicated
Workup to assess for etiology/modifiable risk factors
• Cardiac: Holter to assess for arrhythmias; echo to assess for thrombus or vegetation, w/ bubble study to assess for PFO/atrial septal aneurysm if suspected embolic stroke • Vessel imaging: carotid U/S and Doppler (if no vessel imaging obtained in acute eval) • Labs: lipids, HbA1c, TSH, homocysteine, Lp(a), hypercoag w/u (if <65 y or cryptogenic stroke; ideally drawn before starting anticoag), ESR/CRP, blood cx if s/s systemic infection •
MRI
helpful if dx of stroke unclear (esp. post circ) or to define stroke subtype, age, exact size
DWI
bright/
ADC
dark = earliest finding in acute ischemia (~ w/in mins, up to days)
T2-FLAIR
: hyperintense w/in hrs, persists for wks;
PWI
differentiates irreversibly infarcted core vs. viable penumbra;
T1
fat-sat
(neck vessels) if suspicious for dissection
Acute treatment of ischemic stroke (
NEJM
2011;364:2138;
Stroke
2013;44:870)
•
Thrombolysis (IV)
: tPA 0.9 mg/kg (max 90 mg), w/ 10% as bolus over 1 min, rest over 1 h
consider if onset w/in 4.5 h, ICH, contraindic. (incl. current/prior ICH; head trauma or stroke w/in 3 mo; intracranial neoplasm, AVM or aneurysm; recent intracranial/intraspinal surgery; active internal bleeding; noncompressible arterial puncture; ↑ BP; multilobar infarct; plt <100k, INR >1.7, on Xa inhib, PTT >40, glc <50)
0–3 h: 12% absolute ↑ in good neuro outcome (min/no disability), 5.8% absolute ↑ in ICH, trend toward 4% absolute ↓ mortality
3–4.5 h: 7.2% absolute ↑ in good neuro outcome, 1.8% absolute ↑ in ICH, mortality benefit (nb, trial excluded patients with previous strokes + DM)
tenecteplase 0.25 mg/kg IV bolus promising (
NEJM
2012;366:1099)
Other books
Jihad Joe by J. M. Berger
The Best Place on Earth by Ayelet Tsabari
Execution Style by Lani Lynn Vale
Vengeance 02 - Trust In Me by Lana Williams
A Creepy Case of Vampires by Kenneth Oppel
Alice's Tulips: A Novel by Dallas, Sandra
Night Birds On Nantucket by Joan Aiken
The Nerd Who Loved Me by Liz Talley
Blood To Blood by Ifè Oshun
The Bigness of the World by Lori Ostlund