Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (120 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
3.91Mb size Format: txt, pdf, ePub
•
Migraine
:
see below
Secondary causes of headaches
• Traumatic: postconcussion, SAH, SDH, postcraniotomy • ↑ ICP: mass (tumor, abscess, vascular malformations, ICH), hydrocephalus, idiopathic intracranial hypertension (pseudotumor cerebri), altitude associated cerebral edema • ↓ ICP: post-LP headache, CSF leak/dural tear, overshunting • Vascular causes: stroke (esp. posterior circ), dissection, vasculitis (incl. temporal arteritis), reversible cerebral vasoconstriction syndrome (RCVS), ICH, venous sinus thrombosis • Meningeal irritation: meningitis, SAH
• Trigeminal neuralgia • Extracranial: sinusitis, TMJ syndrome, glaucoma • Systemic causes: hypoxia, hypercapnia, dialysis HA, HTN, hypoglycemia, ↓TSH
• Medication overuse (analgesics), withdrawal (caffeine, opioids, estrogen)
Clinical evaluation (
JAMA
2006;296:1274)
• History: onset (sudden vs. gradual), quality, severity, location, duration, triggers, alleviating factors, positional component, hormonal triggers (menstruation), preceding trauma, associated sx (visual Δs, “floaters,” N/V, photophobia, focal neurologic sx) • Medications (analgesics), substance abuse (opioids, caffeine) • General and neurologic exam (fundoscopic exam, visual fields) •
Warning signs (should prompt neuroimaging)
explosive onset
(vasc);
“worst HA of my life”
(SAH, RCVS);
meningismus
(SAH, infxn)
positional
: lying > standing (↑ ICP);
N/V
(↑ ICP; migraines)
visual sx
: diplopia, blurring, ↓ acuity (GCA, glaucoma, ↑ ICP);
eye pain
(glaucoma, cluster)
abnl neuro exam
(struct. lesion, poss. in migraine); ↓
consciousness
(± fever): infxn, ICH
age
>
50 y
;
immunosuppression
(CNS infections, PRES)
• LP if suspicious for SAH (✓ for xanthochromia), pseudotumor (✓opening press); image first!
MIGRAINE
Epidemiology:
affects 15% of women and 6% of men; onset usually by 30 y
Definition & clinical manifestations (
Lancet
2004;363:381;
JAMA
2006;296:1274)
• H/o ≥5 attacks lasting 4–72 h and with (a) N/V
or
photophobia & phonophobia, and (b) ≥2 of following: unilat., pulsating, mod–severe intensity, aggravated by routine activity • Migraine w/o aura (64%): most common, previously called “common” migraine • Typical aura w/ migraine (18%): visual aura (scotomata with jagged/colored edge) precedes HA, can also be reversible sensory or speech symptoms, <1 h • Complicated: accompanied by stereotypical neurologic deficit that may last hrs (DDx includes
stroke
: in migraine onset is rather gradual, sx spread over mins) • Precipitants: stress, hunger, foods (cheese, chocolate) and food additives (MSG), fatigue, alcohol, menstruation, exercise
Treatment (
NEJM
2002;346:257)
• Eliminate precipitants
• Prophylaxis: TCA, βB, CCB, valproic acid, topiramate (
JAMA
2004;291:965), gabapentin • Abortive therapy: ASA, acetaminophen, caffeine, high-dose NSAIDs
metoclopramide IV, prochlorperazine IM or IV, valproate IV, steroids
5-HT
1
agonists (“triptans”): most specific therapy, contraindicated if complicated migraine, CAD, prior stroke. Triptan + NSAID stronger than either alone (
JAMA
2007;297:1443)
ergotamine, dihydroergotamine: use with caution in Pts w/ CAD
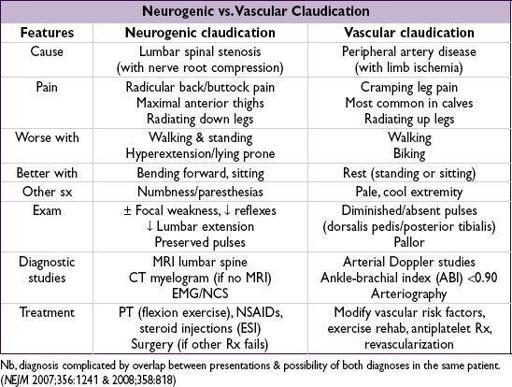
BACK AND SPINAL CORD DISEASE
Differential diagnosis of back pain
•
Musculoskeletal
: musculoligamentous “strain” (experienced by up to 80% of population at some time), OA, RA, spondylolisthesis, vertebral fx, inflammatory spondyloarthritis (ankylosing spondylitis, reactive, psoriatic), myofascial pain syndrome •
Spinal cord
(myelopathy)
/nerve root
(radiculopathy):
Degenerative/traumatic: disc herniation, spondylosis, vertebral fx and subluxation
Neoplastic: lung, breast, prostate, RCC, thyroid, colon, multiple myeloma, lymphoma
Infectious (also see ID section): osteomyelitis, epidural abscess, zoster, Lyme, CMV, HIV
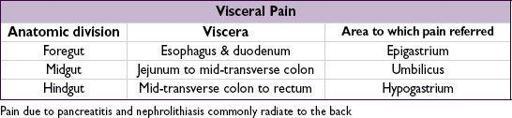
•
Referred pain from visceral disease
: (quality of pain can be important to distinguish)
GI: PUD, cholelithiasis, pancreatitis, pancreatic cancer
GU: pyelonephritis, nephrolithiasis, uterine or ovarian cancer, salpingitis
Vascular: aortic dissection, leaking aortic aneurysm
Initial evaluation
•
History
: location, radiation, trauma, wt loss, cancer hx, fever, immunocompromised, neurologic symptoms, saddle anesthesia, incontinence, urinary retention, IV drug use •
General physical exam
: local tenderness, ROM, signs of infection or malignancy,
signs of radiculopathy (experienced as sharp/lancinating pain radiating into limb):
Spurling sign (radicular pain w/ downward force to extended & ipsilaterally rotated head): 30% Se, 93% Sp
straight leg raise (radicular pain at 30–70°): ipsilateral: 92% Se, 28% Sp; crossed (contralateral leg raised): 28% Se, 90% Sp
•
Neurologic exam
: full motor (including sphincter tone), sensory (including perineal region) and reflexes including anal (S4) and cremasteric (L2) •
Laboratory
(depending on suspicion): CBC, ESR, Ca, PO
4
, AФ, CSF
•
Neuroimaging
: low yield if nonradiating pain, high falserate (incidental spondylosis) depending on suspicion: X-rays, CT or CT myelography, MRI, bone scan •
EMG/NCS
: may be useful to distinguish root/plexopathies from peripheral neuropathies
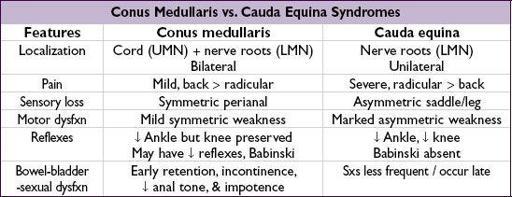
SPINAL CORD COMPRESSION
Clinical manifestations
• Acute: flaccid paraparesis and absent reflexes (“spinal shock”) • Subacute–chronic: spastic paraparesis and hyperactive reflexes • Posterior column dysfunction in legs (loss of vibratory sense or proprioception) • Sensory loss below level of lesion
• Bilateral prominent Babinski responses ± ankle clonus
Evaluation & treatment
• Empiric spine immobilization (collar, board) for all trauma patients • STAT MRI (at and above clinical spinal level, pre-and postgadolinium) or CT myelogram • Emergent neurosurgical and/or neurology consultation • Urgent radiation therapy ± surgery for compression if due to metastatic disease • High-dose steroids depending on cause:
Tumor: dexamethasone 16 mg/d IV (usually 4 mg q6h) with slow taper over wks
Trauma: methylprednisolone 30 mg/kg IV over 15 min then 5.4 mg/kg/h × 24 h (if started w/in 3 h of injury) or × 48 h (if started 3–8 h after injury) (
JAMA
1997;277:1597)
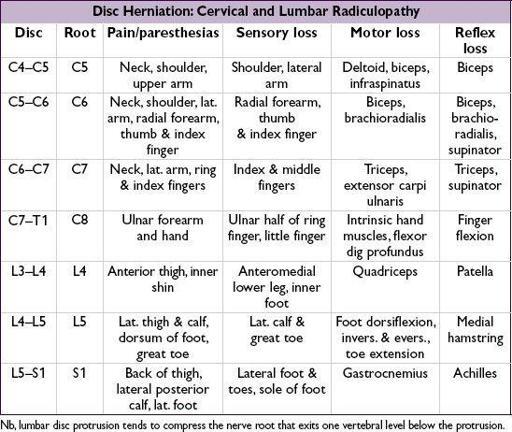
NERVE ROOT COMPRESSION
Clinical manifestations
• Radicular pain aggravated by activity (esp. bending, straining, coughing), relieved by lying • Sciatica = radicular pain radiating from buttocks down lateral aspect of leg, often to knee or lateral calf ± numbness and paresthesias radiating to lateral foot
Treatment of nerve root compression
• Conservative: avoid bending/lifting; NSAIDs; Rx neuropathic pain (see “Peripheral Neuropathies”); physical therapy • Spinal epidural steroid injections (ESI): limited short-term relief of refractory radicular pain • Surgery: cord compression or cauda equina syndrome; progressive motor dysfunction; bowel/bladder dysfunction; failure to respond to conservative Rx (
NEJM
2007;356:2245)
SURGICAL ISSUES
ABDOMINAL PAIN
Other books
Supernatural Fairy Tales by Vann, Dorlana
Doomraga's Revenge by T. A. Barron
Smarty Bones by Carolyn Haines
A Perfect Proposal by Katie Fforde
Corrected by the Colonel by Celeste Jones
Can't Resist a Cowboy by Otto, Elizabeth
Taken by H.M. McQueen
Apocalypse in the Homeland: The Adventures of John Harris by Anthony Newman
The Man to Be Reckoned With by Tara Pammi
Cronin's Key III by N.R. Walker