Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (60 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

Workup
(
Archives
2001;161:25)
•
Acute GN/RPGN
±
lung hemorrhage is an emergency
→ requires early Dx and Rx • ANCA (
Lancet
2006;368:404), anti-GBM, complement levels • Depending on clinical hx: ANA, ASLO, BCx, cryocrit, hepatitis serologies, skin bx • Consider GN mimics
thrombotic microangiopathy: ↓ Hct & Plts, schistocytes on smear, ↑ LDH cholesterol emboli (
Lancet
2010;375:1650): purple toes, livedo, ↓ C3/C4, eos, prior cath AIN: rash, new drug exposure, urine WBCs (incl eos) ± WBC casts (andUCx) myeloma: anemia, hypercalcemia, lytic bone lesions,
SPEP/serum free light chains
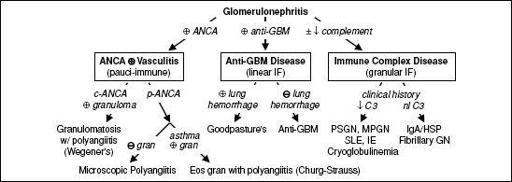
• Renal biopsy with immunofluorescence (IF) ± electron microscopy (EM)
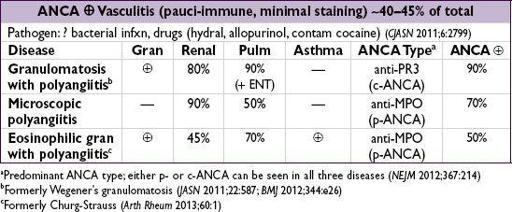
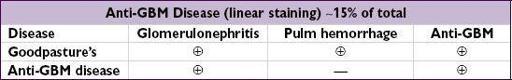
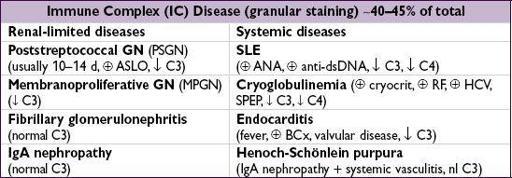
Figure 4-8
Approach to glomerulonephritis
Treatment
(
Kid Int Sup
2012;2:143)
• If acute GN/RPGN suspected, give 1 g methylprednisolone IV qd x 3 d
ASAP
while awaiting bx results, further Rx based on underlying disease (
AJKD
1988;11:449) • SLE nephritis: steroids + cyclophosphamide (CYC) or MMF (
JASN
2009;20:1103) • ANCA or anti-GBM: pulse steroids + CYC (or rituximab) ± plasmapheresis (
or anti-GBM: pulse steroids + CYC (or rituximab) ± plasmapheresis (
JASN
2007;18:2180;
NEJM
2010;363:221) • See “Vasculitis” for further disease specific treatment details
ASYMPTOMATIC GLOMERULAR HEMATURIA
Definition and etiologies
• Hematuria ± proteinuria of glomerular origin w/o renal insufficiency or systemic disease (nonglomerular hematuria more common; see “Hematuria”) • Ddx: any cause of GN (esp. IgA); also consider Alport’s (X-linked, deafness, renal failure), thin basement membrane nephropathy (autosomal dominant, benign;
JASN
2006;17:813)
IgA nephropathy
(
NEJM
2002;347:738;
JASN
2005;16:2088)
• Most common cause of GN; male predominance w/ peak incidence 20–30s • Wide range of clinical presentations: asx hematuria (30–40%), gross hematuria ~1–3 d after URI (30–40%), chronic GN (10%), nephrotic syndrome (5%), RPGN (<5%) • Though clinical presentation can be highly suggestive, definitive dx only w/ bx • Prognosis: 25–30% will reach ESRD w/in 20–25 y of presentation • Treatment: ACEI/ARB, ± fish oils (
JASN
1999;10:1772); steroids (
JASN
2012;23:1108); ± cytotoxic therapy for crescentic GN and nephrotic sx, consider for progressive chronic GN
NEPHROTIC SYNDROME
Definition
(
NEJM
1998;338:1202)
• Proteinuria >3.5 g/d, albumin <3.5 mg/dL, edema, ↑ cholesterol
Primary glomerular diseases
(grouped by pathology)
•
Focal segmental glomerulosclerosis
(40%;
NEJM
2011;365:2398;): 1º (? ↑ soluble urokinase receptor;
Nat Med
2011:17;952), HIV (collapsing variant), NSAIDs, lymphomas, pamidronate, heroin, congenital, ↑ filtration from prior nephron loss, obesity, vesicoureteral reflux, anabolic steroids, genetic (trypanolytic ApoL1 mutation in AA;
Science
2010;329:841) •
Membranous nephropathy
(30%;
JASN
2012;23:1617) idiopathic (phospholipase A
2
receptor Abs;
NEJM
2009;361:11), infxn (esp. HBV, also HCV, syphilis), autoimmune (esp. SLE), carcinomas, drugs (NSAIDs, penicillamine) •
Minimal change disease
(20%, more common in children;
NDT
2003;18:vi52) idiopathic, NSAIDs, Hodgkin’s disease, & other lymphoproliferative disorders •
Membranoproliferative GN
(5%,
mixed
nephrotic/nephritic features;
NEJM
2012;366:1119) Immune complex-mediated: infection (esp. HCV ± cryos, IE, HBV, “shunt” nephritis, other chronic infxns), SLE, cryos, Sjögren’s, lymphomas, dysproteinemia, idiopathic Complement-med (rare); abnl C3 convertase activity, dense deposit dis, C3GN
•
Fibrillary-immunotactoid glomerulopathy
(1%;
Kid Int
2003;63:1450) •
Mesangial proliferative GN
(? atypical forms of MCD/FSGS, 5%) IgM, C1q nephropathy
Systemic diseases
•
Diabetes mellitus
: nodular glomerulosclerosis (Kimmelstiel-Wilson lesion); large kidneys hyperfiltration → microalbuminuria → dipstick→ nephrotic range (10–15 y) concomitant proliferative retinopathy seen in 90% of type 1 and 60% of type 2
•
Amyloidosis
: AL or light chain amyloid or AA amyloid secondary to inflammation •
SLE
: typically with membranous nephropathy (WHO class V) •
Cryoglobulinemia
: typically with membranoproliferative GN
Workup
(
Archives
2001;161:25;
BMJ
2008;336:1185)
• Urine sediment: usually benign; ± oval fat bodies (“Maltese crosses”;
NEJM
2007;357:806) • Measure proteinuria: 24-h urine collection or urine prot/Cr ratio (not accurate in AKI) • r/o 2° causes: ↑ Hb
A1C
+ retinop. → presumpt. dx of diab. nephrop.; ✓ ANA, anti-dsDNA, C3/C4, SPEP/free light chains, fat pad bx, cryocrit, HBV/HCV, HIV, RPR, PLA
2
recept. Ab • Renal biopsy
Treatment
(
Kid Int Sup
2012;2:143;
NEJM
2013;368:10)
• General: protein suppl.; diuretics for edema; treat hyperlipidemia, Na restriction (<2 g/d) •
ACEI
/
ARB
: decrease proteinuria → slow nonimmunologic progression of renal disease • 1° glomerular dis: steroids ± cytotoxic therapy; cancer screening if membranous neph.