Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (65 page)
Read Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine Online
Authors: Marc Sabatine
Tags: #Medical, #Internal Medicine

BOOK: Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine
10.47Mb size Format: txt, pdf, ePub
Etiologies
• ↓
production
hypocellular bone marrow
: aplastic anemia (qv), rarely MDS, drugs (eg, thiazides, antibiotics), alcohol, cirrhosis
hypercellular bone marrow
: MDS, leukemia, severe megaloblastic anemia
marrow replacement
: myelofibrosis, hematologic and solid malignancies, granulomas
• ↑
destruction
immune-mediated
(distinguish primary from secondary;
Blood
2009;113:2386) Primary (idiopathic): immune thrombocytopenic purpura (
ITP
, see below)
Secondary: infxn (
HIV
,
HCV
, HSV), collagen vascular diseases (
SLE
), APS, lymphoproliferative (
CLL
, lymphoma), drugs (
many
, including
heparin
, abciximab, quinidine, sulfonamides, vancomycin), alloimmune (posttransfusion)
non–immune-mediated
:
MAHA
(DIC, HUS, TTP), ticlopidine/clopidogrel, vasculitis, preeclampsia/HELLP, cardiopulm bypass, CVVH, IABP, cavernous hemangioma
•
Abnormal distribution or pooling
: splenic sequestration, dilutional, hypothermia •
Unknown
: ehrlichiosis/anaplasmosis, babesiosis, RMSF
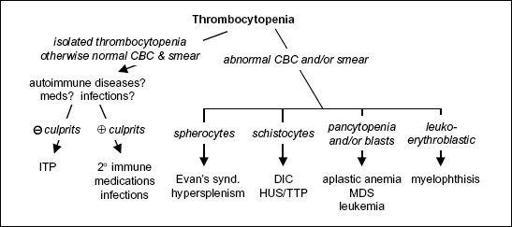
Diagnostic evaluation
• H&P: meds, infxns, underlying conditions, splenomegaly, lymph nodes,
bleeding hx
•
CBC with differential
: isolated thrombocytopenia
vs
. multilineage involvement •
Peripheral smear
↑ destruction → look for large plts,
schistocytes
(see “Peripheral Smear” inserts)
↓ production → rarely limited to platelets → look for
blasts
, hypersegmented PMNs, leukoerythroblastic Ds; can see inclusion bodies (anaplasma), parasites (babesia)
r/o
pseudothrombocytopenia
due to platelet clumping (✓ platelet count in non–EDTA-containing tube, eg, citrate-containing yellow top tube)
Figure 5-5
Approach to thrombocytopenia
• Additional laboratory evaluations as indicated (eg, viral titers, flow cytometry, ANA, APLA)
if anemia: ✓ reticulocyte count, LDH, haptoglobin, bilirubin to detect hemolysis
if hemolytic anemia: ✓ PT, PTT, fibrinogen, D-dimer, Coombs, ANA
BM bx for unexplained thrombocytopenia, esp. if associated with splenomegaly
Primary immune thrombocytopenic purpura (ITP)
(
Blood
2010;115:168)
• Primary ITP: isolated thrombocytopenia due to immune plt
destruction
& ↓
production
(auto-Ab to megakaryocytes); (2° ITP a/w disease/drug exposure; Rx underlying disorder) • Primary ITP is
diagnosis of exclusion
; no robust clinical or lab parameters, but typically:
CBC: isolated ↓ plt (<100,000/µL); 10% have ITP + AIHA = Evans syndrome
Peripheral smear: large platelets
BM bx: ↑ megakaryocytes; perform in adults >60 y to r/o myelodysplasia
R/o other etiologies
: viral serologies (
HIV
,
HCV
, HBV, EBV),
H. pylori
Ab, ANA, pregnancy test, APLA, TSH, parvovirus, & CMV PCR.
Anti-plt Ab tests not useful
.
• Clinical manifestations: insidious onset of mucocutaneous bleeding;:
= 3:1
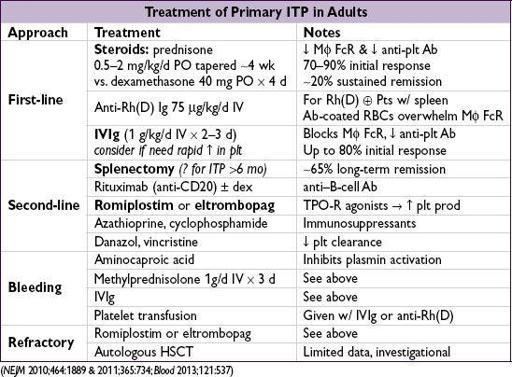
• Treatment: goals based on individual Pt rarely indicated if plt >50,000/µL unless bleeding, trauma/surgery, anticoag, comorbidities
steroids
,
IVIg
, & splenectomy mainstay of initial Rx; romiplostim/eltrombopag if refractory
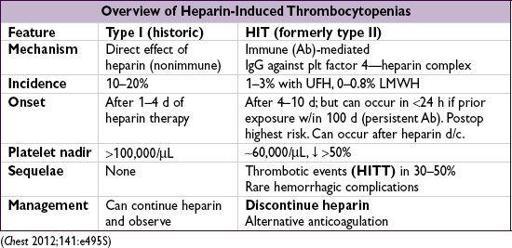
• Pathophysiology (type II): Ab binds heparin-PF4 → immune complex binds to plt →
plt activation
, further PF4 release → plt aggregates removed from circulation →
thrombocytopenia
; procoagulants released by plts and tissue factor released by endothelial cells damaged by HIT Abs →
prothrombotic state
• Diagnosis
(need clinical
+
pathologic)
Clinical
: plt <100k
or
↓ 50% from baseline; or
venous
(DVT/PE) or
arterial
(limb ischemia, CVA, MI) thrombosis (4:1 ratio); skin necrosis; ? ↑ heparin resistance
Pathologic
:HIT Ab using PF4-heparin ELISA (≥90% Se, IgG-specific ELISA Sp 94%), may confirm w/ functional plt aggregation (serotonin-release) assay (>90% Sp)
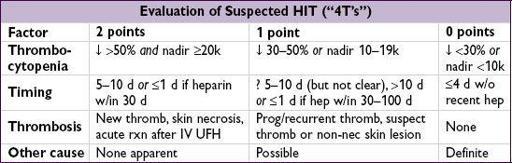
Pretest prob w/ “4T’s” criteria (
Blood
2012;120:4160): ≤3 points → 99% NPV, investigate other causes; 4–5 points 22% PPV & 6–8 points 64% PPV, ✓ lab test and replace UFH
• Treatment of HIT (type II) (
Chest
2012;141:e495S;
Blood
2012;119:2209;
NEJM
2013;368:737)
Discontinue heparin
(including flushes, LMWH prophylaxis, heparin-impregnated lines)
Avoid plt transfusions if not actively bleeding (anecdotally linked w/ thrombotic events)
Nonheparin anticoag
(argatroban, bivalirudin;
NEJM
2013;368:737)
regardless of thrombosis
; start warfarin when plt >150k, overlap ≥5 d (✓ chromogenic Xa to titrate)
thrombosis (HITT): anticoagulate for ≥ 3–6 mo
Other books
La comunicación no verbal by Flora Davis
Truants by Ron Carlson
Wildfire by Cathie Linz
The Princes of Tangleforest by Vann, Dorlana
Kate by Claudia Joseph
Where Love Shines by Donna Fletcher Crow
Rise of the Faire-Amanti (The Ascendant Series Book 3) by Raine Thomas
Angelmaker by Nick Harkaway
Holding Their Own VII: Phoenix Star by Nobody, Joe
Corvus by Paul Kearney