The Washington Manual Internship Survival Guide (17 page)
Read The Washington Manual Internship Survival Guide Online
Authors: Thomas M. de Fer,Eric Knoche,Gina Larossa,Heather Sateia
Tags: #Medical, #Internal Medicine

•
In the stable patient, a WCT can be the result of a supraventricular rhythm (including sinus tachycardia) with bundle branch block, a supraventricular rhythm with aberrant conduction, or ventricular tachycardia (VT).
Diagnosis of WCT
•
Key features on history, labs, and the ECG can help make the diagnosis.
•
In a patient with structural heart disease, history of MI, or significant abnormalities of magnesium or potassium levels, a WCT is almost always VT, given that the patient does not have underlying bundle branch block
(
Figure 19-4
).
•
The presence of capture or fusion beats on ECG clinches a diagnosis of VT as well.
•
There have been numerous proposed algorithms to aid in the diagnosis of WCT as supraventricular tachycardia versus VT, the most well-known of which is the Brugada Criteria, found elsewhere.
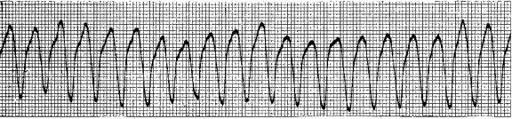
Figure 19-4.
Ventricular tachycardia.
•
Remember,
in a patient with chest pain and a new WCT, acute MI is a very likely diagnosis
, and you should immediately instruct the nurse to administer aspirin and call for help!
Management of WCT
•
Management of stable WCT depends on the diagnosis.
•
In the case of VT, options include electrical cardioversion or attempted pharmacologic cardioversion.
•
In the case of SVT, management is per the NCT section above.
•
In either case, the patient is at high risk for something bad happening and you should call for help before initiating treatment!
Nonsustained Ventricular Tachycardia
•
Often as an intern, you will be called for “beats of NSVT” or “run of NSVT.”
•
NSVT, or nonsustained ventricular tachycardia, is defined as fewer than 30 consecutive wide-complex beats that are ventricular in origin.
•
These usually occur in patients with heart failure or toxin ingestion. Given that these patients are usually hemodynamically stable, nothing need be done on an emergent basis.
•
As always, if the patient demonstrates hemodynamic instability or altered mental status during the episodes, ask for help, as the patient likely requires treatment.
•
Large studies have been done to evaluate the outcomes for patients who are treated with antiarrhythmic agents to suppress ectopic beats. In these studies, those patients whose ectopic beats were effectively suppressed had higher mortality, whereas those simply treated with β-blockade had improved survival.
•
Therefore, in most patients with NSVT, titrating up a β-blocker as tolerated is currently the most effective management.
•
NSVT alone is rarely an indication for placement of an intracardiac cardioverter-defibrillator (ICD).
Ventricular Fibrillation and Torsades de Pointes
•
Close this book and call a Code Blue!
These rhythms should prompt immediate initiation of ACLS and rapid defibrillation.
•
In the case of torsades, IV magnesium can aid restoration of normal sinus rhythm.
BRADYARRHYTHMIAS AND DISORDERS OF CONDUCTION
Sinus Bradycardia
•
Sinus bradycardia is defined as sinus rhythm with a rate of less than 60 bpm.
•
Sinus bradycardia is most often caused by increased vagal tone, antiarrhythmic agents, ischemia, and conduction system degeneration
(with long-standing hypertension, diabetes, or increased age).
•
Sinus bradycardia is common in sleeping patients.
•
Sinus bradycardia should be
treated only if symptoms of hypotension exist
. That is to say, if you are called for sinus bradycardia, and the patient is asymptomatic with an acceptable blood pressure, this patient requires no treatment.
•
Look for offending agents that can cause bradycardia, such as β-blockers, calcium channel blockers, digoxin, or other medications. Discontinue these immediately.
•
Acute treatment can consist of the anticholinergic agent atropine and/or placement of defibrillator pads with transcutaneous pacing.
•
Atropine can be given in increments of 0.5 mg IV until the heart rate is satisfactory.
•
Atropine has a half-life of 2 hours, so after resolution with atropine, care must be taken to ensure the bradycardia does not return.
•
Infusions such as dopamine or isoproterenol can be considered as pharmacologic means to restore and maintain the heart rate. Call for help prior to initiating these treatments.
•
Transcutaneous pacing should be employed if necessary, but is exceedingly uncomfortable for the patient. Transvenous pacing should be considered in the symptomatically bradycardic patient, with the help of an upper level resident or cardiology fellow.
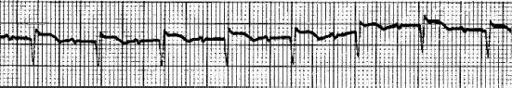
Figure 19-5.
First-degree AV block.
First-Degree AV Block
•
The PR interval is greater than 200 ms, but all p-waves result in a QRS complex (
Figure 19-5
).
•
First-degree block can be caused by increased vagal tone, electrolyte abnormalities, conduction system degeneration, and drugs (calcium channel blockers, β-blockers, and other antiarrhythmic agents are common causes). Ischemia can in specific instances prolong the PR interval.
•
First-degree block rarely requires treatment. If severe, consideration can be given to discontinuation of offending drugs.
Mobitz Type I and Mobitz Type II Second-Degree AV Block
In second-degree block, not all p-waves result in a QRS complex.
Mobitz Type I Block (Wenckebach)
•
Mobitz I is identified when the
PR interval progressively increases
between PQRS complexes, until a p-wave is not conducted to the ventricle and does not result in a QRS complex (
Figure 19-6
).
•
Mobitz I usually occurs as a result of slowed conduction within the AV node.
•
The QRS complexes should not change in morphology.
•
Etiologies are the same for first-degree block.
•
Mobitz type I block is usually asymptomatic.
•
Given that it is asymptomatic, and
does not usually progress to worsening heart block, this type of block requires no treatment
.
•
If symptomatic bradycardia ensues, treatment is the same as that for sinus bradycardia.
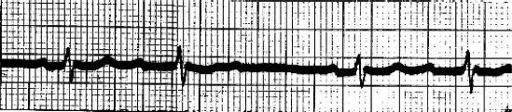
Figure 19-6.
Mobitz type I (Wenckebach), second-degree AV block.
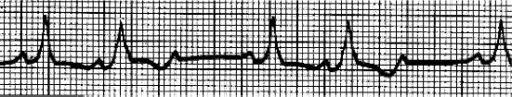
Figure 19-7.
Mobitz type II, second-degree AV block.
Mobitz Type II Block
•
Mobitz type II block is diagnosed when
the PR interval is fixed, but one or more p-waves do not result in a QRS complex
(
Figure 19-7
).
•
Mobitz II usually occurs as a result of slowed conduction just below the AV node.
•
Blocked conduction may occur in a fixed ratio (two, three, or four conducted p-waves for one nonconducted p-wave).
•
Causes are similar to Mobitz type I block.
•
Because Mobitz type II block is at high risk for degenerating into complete AV block, these patients must be closely monitored.
•
Treatment usually involves placement of an external pacemaker, regardless of symptoms.
Third-Degree (Complete) AV Block
•
No p-waves are conducted; complete AV dissociation occurs
(
Figure 19-8
).
•
QRS complexes that arise do so as the result of intrinsic pacemakers within or below the level of the AV node.
•
“Escape” rhythms usually occur in the acute setting that obviate the development of asystole. If a narrow QRS occurs, the rhythm originates from the AV node’s intrinsic pacemaker and is referred to as “junctional.” If a wide QRS occurs, the rhythm originates from somewhere within the ventricles and is termed “idioventricular.”
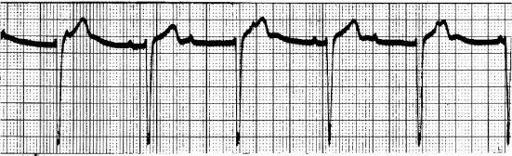
Figure 19-8.
Complete heart block.
•
Third-degree block carries a high risk of degeneration to asystole
.
•
Therefore, regardless of symptoms, an immediate plan for
transcutaneous and/or transvenous pacer
, with eventual permanent pacemaker, should be implemented.