Examination Medicine: A Guide to Physician Training (48 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

Investigations
To support the diagnosis (remembering that this is primarily a clinical diagnosis; see
Table 9.2
), investigations include:
Table 9.2
Criteria for the diagnosis of rheumatoid arthritis in newly presenting cases (2010 ACR/EULAR RA criteria)
| Target population (Who should be tested?): patients who: 1. have at least one joint with definite clinical synovitis (swelling) 2. with the synovitis not better explained by another disease |
| CLASSIFICATION CRITERIA FOR RA | SCORE |
| (score-based algorithm: add score of categories A–D; a score of ≥6/10 is needed for classification of a patient as having definite RA) | |
| A. JOINT INVOLVEMENT | |
| 1 large joint | 0 |
| 2–10 large joints | 1 |
| 1–3 small joints (with or without involvement of large joints) | 2 |
| 4–10 small joints (with or without involvement of large joints) | 3 |
| >10 joints (at least one small joint) | 5 |
| B. SEROLOGY (AT LEAST ONE TEST RESULT IS NEEDED FOR CLASSIFICATION) | |
| Negative RF and negative ACPA | 0 |
| Low-positive RF or low-positive ACPA | 2 |
| High-positive RF or high-positive ACPA | 3 |
| C. ACUTE-PHASE REACTANTS (AT LEAST ONE TEST RESULT IS NEEDED FOR CLASSIFICATION) | |
| Normal CRP and normal ESR | 0 |
| Abnormal CRP or abnormal ESR | 1 |
| D. DURATION OF SYMPTOMS | |
| <6 weeks | 0 |
| ≥6 weeks | 1 |
| ACPA = anti-citrullinated protein antibody; RF = rheumatoid factor | |
© 2010 American College of Rheumatology and European League Against Rheumatism. Rheumatoid Arthritis Classification Criteria 2010.
Arthritis and Rheumatism
, 62(9):2569–2581, 2010.
1.
serological tests
a.
rheumatoid factor – 70% of patients are seropositive; patients may at first be seronegative and seroconvert later. (
Note:
Most patients are rheumatoid factor positive if they have nodules or associated vasculitis; remember that more than 10% of well people over the age of 65 have rheumatoid factor and that it is commonly found in association with infections and other inflammatory conditions, in relatives of patients with rheumatoid arthritis and transiently after some vaccinations.)
b.
anti-citrullinated cyclic peptide (anti-CCP) – this is more specific (97%); it is associated with a more severe disease course and erosive disease
2.
X-ray films of involved joints
– changes to look for are:
a.
soft-tissue swelling
b.
symmetrical joint space narrowing (OA causes asymmetrical narrowing) (
Figs 9.2
and
9.3
)
FIGURE 9.2
Cervical spine X-ray of a patient with rheumatoid arthritis. Note the erosions and loss of joint space. Special views are needed to exclude erosion of the odontoid process. Figure reproduced courtesy of The Canberra Hospital.
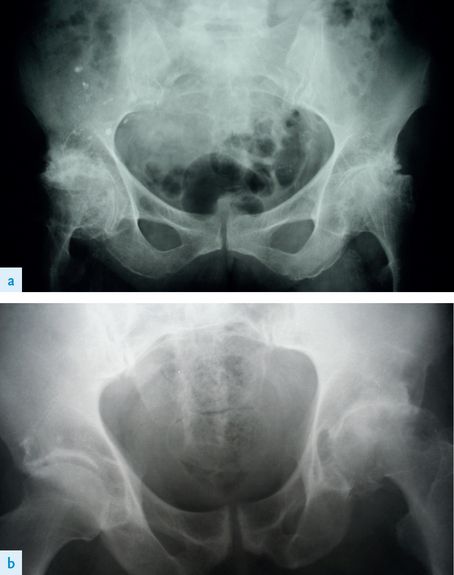
FIGURE 9.3
(a) X-ray of the pelvis of a patient with rheumatoid arthritis. Note the severe destructive changes on both sides – very different from (b). (b) Osteoarthritis (OA) of the left hip. Note the asymmetrical loss of joint space. Figures reproduced courtesy of The Canberra Hospital.
c.
juxta-articular osteoporosis
d.
marginal joint erosions (
Fig 9.4
).
FIGURE 9.4
X-ray of the chest of a patient with rheumatoid arthritis involving the shoulder. Note the erosions of the humeral heads with subluxation and erosions of the distal clavicles. Figure reproduced courtesy of The Canberra Hospital.
Investigations used to assess the activity of the disease include:
1.
ESR or CRP – remember that the differential diagnosis of a raised ESR in rheumatoid arthritis includes:
a.
active disease
b.
amyloidosis
c.
infection
d.
Sjögren’s syndrome
2.
haemoglobin measurement – the severity of normochromic anaemia usually correlates with activity
3.
anti-CCP, and rheumatoid factor titres
4.
the presence of progressive erosions on serial X-ray films.
Treatment
1.
Remember that the aim of modern treatment is to induce complete remission of the disease by suppressing the inflammatory process. This means early diagnosis and introduction of disease modifying antirheumatic drugs (DMARDs). The traditional DMRDs will control the disease effectively for many patients, but the newer biological therapies allow many more patients to have the disease controlled. The general principles of treatment include:
•
education
•
physiotherapy, including exercise and splinting of the joints to prevent deformity
•
occupational therapy
•
drug treatment aimed at reducing pain and inflammation (with aspirin, other NSAIDs or COX-2 inhibitors) and at preventing progression of the disease. The gastrointestinal toxicity of the traditional NSAIDs (i.e. peptic ulceration) is reduced by the COX-2 inhibitors; however, all can cause dyspepsia and renal disease (e.g. acute interstitial nephritis) and worsen renal function in patients with diabetic or atherosclerotic kidney disease; all NSAIDs are associated with an increased risk of myocardial infarction. If there is aspirin allergy, sodium salicylate is an alternative.
2.
The use of DMARDs is now recommended early on for patients with active progressive disease, especially if there is evidence of joint destruction (see
Table 9.3
). These drugs include methotrexate, sulfasalazine, hydroxychloroquine, cyclosporin, leflunomide, azathioprine, penicillamine and gold (oral or injected). These medications have a slow onset of action (weeks for methotrexate to months for gold). There is evidence that they can lead to healing of bone erosions. Monitoring should include full blood count, urine testing for proteinuria and specific tests for certain drugs, such as liver function tests for methotrexate, or ophthalmological examination and assessment of visual fields for hydroxychloroquine.
Table 9.3
Risk factors for destructive disease

3.
Methotrexate is the most commonly used of these drugs; it can be given orally or intramuscularly, usually 10–25 mg weekly, but starting with a low dose. It is usually better tolerated than the other DMARDs and is often the drug of first choice and given early in the course of the disease to decrease inflammation and sometimes the development of synovitis. Methotrexate may sometimes cause an increase in the number of rheumatoid nodules. It can be given alone or in combination with hydroxychloroquine and sulfasalazine. Folic acid is given daily to decrease the risk of side-effects of methotrexate, especially mouth ulcers. Safety monitoring includes full blood count and liver function tests. Adverse reactions include rash, abnormal liver function tests (transaminases), leucopenia, thrombocytopenia and interstitial lung disease. It should not be given to patients with glucose-6-phosphate dehydrogenase deficiency.
4.
Alternative agents in use include leflunomide (a pyrimidine antagonist that inhibits the proliferation of T cells).
5.
The biological agents are generally second-line treatments because of their cost but their use has increased greatly recently.
Table 9.4
shows the current prescribing rules for these drugs, while
Table 9.5
lists their side-effects and precautions for their use.
Table 9.4
Rules for use of biological agents for the treatment of rheumatoid arthritis