Examination Medicine: A Guide to Physician Training (51 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

10.
Mycophenalate and a number of new biological agents are being tested in clinical trials. Autologous stem cell transplant is also an experimental treatment.
11.
Remember that postpartum exacerbations of lupus may occur. Spontaneous abortions are common in women with antiphospholipid antibodies. Treatment with anticoagulation (heparin plus low-dose aspirin – never prescribe warfarin) may be effective in reducing the risk of abortion. Steroids may be used in pregnancy because, except for dexamethasone, these do not cross the placenta. Women with the anti-Ro (SSA/SSB) antibody may have babies with permanent complete heart block and transient erythematous rashes.
Systemic vasculitis
Patients with a systemic vasculitic illness will often be used for the long-case examination because of the complex nature of these illnesses and the frequent need for hospitalisation. The fact that these illnesses tend to affect multiple body systems across numerous specialties is ideal to test candidates’ general approach to internal medicine. The majority of cases seen in the examination will have a vasculitis such as Wegener’s granulomatosis, giant cell arteritis or polyarteritis nodosa. Occasionally, less common adult vasculitides, such as Churg-Strauss syndrome or microscopic polyarteritis, will be encountered.
The long-case examination for the patient with systemic vasculitis requires the candidate to take a careful history and examine the patient in a thorough general manner, as well as look for specific abnormalities in each disease. Candidates will be expected to have a good knowledge of the various investigative tools available to diagnose vasculitis. The course of treatment will invariably be discussed in this type of case, particularly the side-effects of long-term medications and likely prognosis.
The history
In most cases, the onset of a systemic vasculitic illness is subacute rather than acute. The patient has often seen several practitioners before a diagnosis is made. The history will be critical in determining the diagnosis if the patient has a systemic vasculitis and presents a diagnostic problem, or indeed if there are significant management issues.
1.
First, ask about the systemic features that would suggest a vasculitic illness: fatigue, malaise, fever, myalgia and arthralgia will be very frequent in these patients. Ask about vasculitic skin rash, which would normally be in the form of palpable purpura. Ask about the pattern of joint involvement.
2.
Next ask about a history of renal disease, particularly hypertension or renal failure, and any gastrointestinal symptoms.
3.
Wegener’s granulomatosis
(small or medium-sized vessels, venules and capillaries causing a pulmonary–renal syndrome): the upper and lower respiratory tract are almost invariably involved and frequent symptoms include:
•
nasal congestion
•
rhinorrhoea
•
bloody nasal discharge
•
cough (which is initially a dry cough, but may evolve into haemoptysis)
•
breathlessness.
4.
Giant cell arteritis:
patients are generally in the sixth, seventh or eighth decade of life. About 20% of patients with polymyalgia rheumatica develop giant cell arteritis. The usual specific symptoms are:
•
severe bitemporal headache
•
less commonly, visual disturbance (e.g. diplopia) or visual loss
•
jaw claudication (quite specific), scalp tenderness or occasionally tongue claudication. Other focal neurological symptoms can also occur.
5.
Polyarteritis nodosa
(medium-sized arteries): the specific symptoms depend on which arteries are involved – coronary arteries, mesenteric arteries or renal arteries. Suspect this possibility if there are multiple systems involved (e.g. foot drop with chest and abdominal pain). Ask about risk factors for hepatitis B (one-third of cases).
6.
Churg-Strauss vasculitis
(small vessels causing a pulmonary–renal syndrome): patients almost invariably have asthma first, then a peripheral eosinophilia. Ask about a previous history of:
•
asthma
•
allergic rhinitis, nasal polyps
•
eczema
•
cough and breathlessness
•
peripheral nervous system disease, either in the form of symmetrical peripheral neuropathy or mononeuritis multiplex.
7.
Microscopic polyarteritis
(small vessels causing a pulmonary–renal syndrome): the major problem is usually with renal impairment and lung disease, which may not have any specific symptoms. Systemic symptoms of vasculitis are generally very prominent.
8.
Mixed essential cryoglobulinaemia
(small vessels due to rheumatoid factor bound to IgG): patients present with:
•
palpable purpura of the extremities
•
Raynaud’s disease
•
arthritis
•
neuropathy.
Hepatitis C is common.
The examination
1.
The patient with systemic vasculitis usually looks unwell. Check for fever, sinus tachycardia, pallor and signs of recent weight loss.
2.
Look for livedo reticularis (a net-like pattern – see
Fig 9.8
). The differential diagnosis includes cholesterol atheroembolism after a vascular procedure, antiphospolipid syndrome and vasculitis. Other mimics of vasculitis include atrial myxoma, bacterial endocarditis and thrombotic thrombocytopenic purpura (TTP).
FIGURE 9.8
Livedo reticularis and erythematous macules of the forearms. J Dion. Livedo reticularis and erythematous macules of the forearms indicating cutaneous microscopic polyangitis.
American Journal of Medicine
, 2010. 123(11), with permission.
3.
Other physical signs will be more specific to the actual underlying illness:
•
Wegener’s granulomatosis:
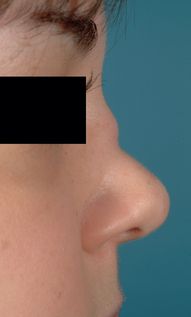
look for the classical collapse of the nasal septum (a saddle-shaped nose (
Fig 9.9
), which also occurs in relapsing polychondritis). There may be evidence of tachypnoea and crackles throughout the lung field. Fluid overload may occur in the setting of worsening renal failure.
FIGURE 9.9
Saddle-shaped nose deformity in Wegener’s. H S Bennett. Restylane – a temporary alternative for saddle nose deformity in nasal Wegener’s granulomatosis – how we do it.
British Journal of Oral and Maxillofacial Surgery
, 2010. 49(4), with permission.
•
Giant cell arteritis:
tender and indurated temporal arteries will often be present. There may be abnormal eye signs if there is retinal involvement. Focal neurological signs should be sought.
•
Polyarteritis nodosa:
there may be evidence of painful skin nodules in rare cases, as well as palpable purpura and livedo reticularis. Look for mononeuritis multiplex.
•
Churg-Strauss vasculitis:
look for signs of allergic disease, such as swollen nasal turbinates, nasal polyps and evidence of bronchospasm. Examine the peripheral nervous system carefully, looking for single nerve lesions or symmetrical peripheral neuropathy generally affecting the lower limbs.
•
Microscopic polyarteritis:
urinalysis is the key – look for any evidence of proteinuria or haematuria.
•
Mixed essential cryoglobulinaemia:
look for Raynaud’s disease, palpable purpura and peripheral neuropathy. Assess for signs of liver disease (hepatitis C).
Investigations
Investigations will be critical in determining the diagnosis in systemic vasculitis.
1.
In most cases a biopsy of affected tissue is the most reliable way of making the diagnosis; other investigations will raise the suspicion that vasculitis is the problem and direct the clinician to a suitable biopsy site.
2.
It will often be necessary to exclude systemic infection, malignancy or generalised autoimmune disease.
3.
In vasculitis, the ESR is invariably raised, often at levels of >70 mm/h. There is frequently a normochromic normocytic anaemia and there may be neutrophilia. The platelet count may be elevated.
4.
Renal function will often be impaired in Wegener’s granulomatosis, polyarteritis nodosa and microscopic polyarteritis.
5.
Abnormal liver function tests, particularly elevated transaminase levels, may be found in Wegener’s granulomatosis and in polyarteritis nodosa. Liver function abnormalities are also reported in giant cell arteritis.
6.
Urine abnormalities will often be found in the form of urinary casts and the presence of dysmorphic red blood cells in the urine, particularly in Wegener’s granulomatosis, microscopic polyarteritis and polyarteritis nodosa.
7.
The chest X-ray will often show a bilateral diffuse interstitial abnormality in Wegener’s granulomatosis (see
Fig 16.31a and b
) and a peripheral fluffy, patchy infiltrative pattern in Churg-Strauss vasculitis.
8.
Wegener’s granulomatosis:
the critical investigation is the antineutrophil cytoplasmic antibody (c-ANCA). This will be present in a vast majority of cases of Wegener’s granulomatosis. Further testing of this antibody will reveal the presence of anti-pr3 antibodies. The presence of a typical clinical syndrome with a positive c-ANCA and pr3 antibodies is virtually diagnostic of Wegener’s granulomatosis. The need for a tissue biopsy may be avoided if these tests are positive. Occasionally, patients with upper airways disease only will not have a positive c-ANCA test.
9.
Giant cell arteritis:
diagnosis depends on a positive tissue sample. Don’t delay starting steroids to make a definite diagnosis (the biopsy can be done within 2 weeks of starting steroids). Temporal artery biopsy should reveal the diagnosis as long as a generous biopsy is taken by the surgeon, but the artery on the other side may need to be sampled in some cases.
10.
Polyarteritis nodosa:
tissue samples are often not available. Many organs may be involved (
Table 9.13
). If symptoms or signs point this way, a biopsy of nerve, muscle or testis may be diagnostic; renal biopsy is not helpful. Angiography is sometimes helpful in this illness, particularly of the mesenteric arteries, but possibly also of the coronary arteries. Bead-like aneurysmal dilation of the arteries is suggestive of polyarteritis.
Table 9.13
Clinical findings in patients with polyarteritis nodosa
| SITE | CLINICAL PROBLEM | PREVALENCE |
| Muscles and joints | Myalgia, arthritis | 65% |
| Kidneys | Hypertension, renal impairment | 60% |
| Gut | Nausea, vomiting, abdominal pain, bowel, liver or pancreatic infarcts | 45% |
| Peripheral nervous system | Mononeuritis multiplex, peripheral neuropathy | 50% |
| Central nervous system | Strokes and seizures | 25% |
| Skin | Purpura, infarcts, Raynaud’s phenomenon | 40% |
| Heart | Cardiac failure, infarction, pericarditis | 35% |
| Genitourinary | Ovarian, testicular pain or infarction | 20% |