Pediatric Primary Care (105 page)

7. Neoplastic such as osteoid osteoma (hallmark sign: night pain or constant pain independent of motion).
8. Other: sickle cell crisis, functional illness, referred pain such as kidney infection or menstrual cramping.
G. Treatment.
1. Depends on diagnosis: rest, nonsteroidal anti-inflammatory drugs (NSAIDs), stretching, abdominal strengthening, proper posture and backpack use, or referral to orthopedist.
H. Follow up.
1. Symptoms should improve in 2 weeks for overuse or strains.
I. Complications.
1. Missed diagnosis (see Differential Diagnosis).
J. Education.
1. Demonstrate exercises to help ensure that they are done correctly.
2. Work with family on medication schedule.
3. If symptoms persist or new symptoms occur, call healthcare provider.
IV. SCOLIOSIS
| Embryonic malformation, 759.9 |
A. Abnormal lateral curvature of spine, typically with vertebral rotation.
B. Etiology.
1. Idiopathic: 90% (most common), unknown etiology, familiar pattern has been noted.
C. Occurrence.
1. Idiopathic: 3–5% in adolescents screened; males = females.
2. 0.6% require treatment; however, females are treated more often (1%) than males (0.1%).
D. Clinical manifestations.
1. Does not typically cause back pain.
E. Physical findings.
1. Difficulty with fitting clothes.
2. S- or C-shape curve of spine.
3. Prominent: scapular, ribcage, paraspinal musculature (especially on forward bend test) or breast.
4. Asymmetric waistline or shoulder level.
5. Plumb line dropped from C-7 does not correlate with gluteal crease.
F. Diagnostic tests.
1. Inspection with minimal clothing.
2. Radiographs: scoliosis series, which is standing postero-anterior (PA) and lateral views of entire spine on one cassette.
G. Differential diagnosis.
| Cerebral palsy, 343.9 | Neurofi bromatosis, 237.7 |
| Emotional disturbance, 313.9 | Polio, 045.1 |
| Muscular dystrophy, 359.1 | Spina bifi da, 741.9 |
| Myopathies, 359.9 | Vertebra fracture, 805.8 |
1. Congenital: embryonic malformation.
2. Paralytic: polio, muscular dystrophy, cerebral palsy, spina bifida, myopathies, neurofibromatosis.
3. Traumatic: fracture of vertebrae.
4. Hysterical: rare, nonstructural, result of emotional disturbance.
H. Treatment.
1. Orthopedic referral all curves > 10°.
2. Orthopedic treatment for curves 10–20° observation.
3. Curves 20–40°: bracing (controversial) to prevent further curvature.
4. Curves > 40°: surgical intervention, posterior spinal fusion with segmental instrumentation occasionally requires anterior release.
I. Follow up.
1. Per orthopedics: until skeletal maturity (about 1 year after menstruation for girls).
J. Complications.
| Lumbar back pain, 724.2 |
1. Progressive untreated scoliosis may result in significant deformity, cardiopulmonary compromise, debilitating lumbar back pain.
K. Education.
1. If braces and/or exercises ordered, ensure compliance.
2. Bracing helps delay progression of curve.
3. Frequent skin inspection necessary with brace use.
4. Continue usual activities if pain free in brace.
V. HIP PAIN
| Hip pain, 719.45 |
A. Differential diagnosis.
1. Infection: septic arthritis, osteomyelitis, Lyme disease, psoas abscess, appendicitis.
2. Inflammatory: transient synovitis, systemic arthritis, juvenile rheumatoid arthritis (JRA), Kawasaki disease, idiopathic chondrolysis.
3. Orthopedic conditions: Legg-Calvé-Perthes disease, avascular necrosis (AVN), slipped capital femoral epiphysis (SCFE), stress fracture, apophyseal injuries, trochanteric bursitis, muscular strain.
4. Neoplastic: osteoid osteoma, leukemia, solid tumor primary, pigmented villonodular synovitis (PVNS), or sickle cell crisis pain.
VI. SEPTIC HIP/SEPTIC ARTHRITIS
| Appendicitis, 541 | Psoas abscess, 015 |
| Avascular necrosis, 733.4 | Septic arthritis, 711 |
| Chondrolysis, 733.99 | Sickle cell crisis, 282.6 |
| Juvenile rheumatoid arthritis, 714.3 | Slipped capitol femoral |
| Kawasaki disease, 446.1 | epiphysis, 732.2 |
| Legg-Calvé-Perthes disease, 732.1 | Systemic arthritis, 716.9 |
| Leukemia, 208.9 | Transient synovitis, 727 |
| Lyme disease, 088.81 | Trochanteric bursitis, 726.5 |
| Muscular strain, 848.9 | Fever, 780.6 |
| Osteoma, 213.9 | Hip pain, 719.45 |
| Osteomyelitis, 730.2 | Septic arthritis hip, 711.08 |
| Pigmented villonodular synovitis (PVNS), 719.2 | |
A. Infection in joint; hip joint is infected often, second only to knee in children.
B. Etiology.
1. Bacterial infection spread hematogenously or from osteomyelitis of the femoral head.
2. Most common organisms are
Staphylococcus
and
Streptococcus.
C. Occurrence.
1. Males = females; infancy to 6 years.
D. Clinical manifestations.
1. Hip pain.
2. Refusal to bear weight.
3. Fever.
4. Ill-appearing child with extreme pain and resistance to hip motion. Infection builds up pressure in hip capsule and can impede blood flow.
E. Physical findings.
1. Fever > 37°C, typically lie with hip flexed and externally rotated.
2. Infants may be irritable with pseudoparalysis of lower extremity.
F. Diagnostic tests.
1. Elevate white blood cells (WBC) and ESR.
2. Ultrasound or radiographs demonstrate widening of joint space.
3. Diagnosis confirmed with CT or ultrasound-guided aspiration.
G. Differential diagnosis.
| Septic sacroiliac joint, 711.08 |
1. Septic sacroiliac joint.
H. Treatment.
1. Emergent referral to hospital for surgical drainage of hip joint.
2. Intravenous antibiotics tailored to culture results.
3. Make sure child receives nothing by mouth (NPO).
I. Follow up.
1. Per orthopedics, usually 1–2 weeks postop and 3–6 months to follow hip maturity.
J. Complications.
| Joint destruction, 718.9 |
| Osteomyelitis, 730.2 |
| Septicemia, 038.9 |
1. Septicemia, osteomyelitis, joint destruction.
K. Education.
1. Prepare family for child's hospitalization and treatment with IV antibiotics.
VII. DEVELOPMENTALLY DISLOCATED HIP
| Breech birth, 763 |
| Dislocated hip, 835 |
| Hip dysplasia, 755.63 |
A. Broad spectrum of hip dysplasia regarding dislocated or dislocatable or subluxing femoral head in relation to acetabulum at birth or early development.
B. Etiology.
1. Genetic, intrauterine position, postnatal positioning.
C. Occurrence.
1. Most common hip disorder in children.
2. 1 in 100 infants have hip instability at birth and true dislocation is seen in 1 of 1000 births.
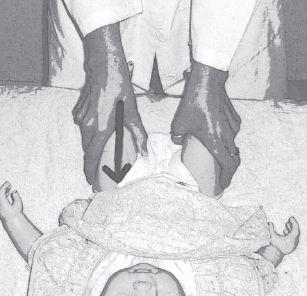
Figure 30–3
Barlow maneuver: knees flexed and brought to midline with gentle downward pressure to see if hip “clunks” out posteriorly.
Other books
A Dark Beginning: A China Dark Novel by Paula Hawkes
Mists of Everness (The War of the Dreaming) by Wright, John C.
Erotic Deception by Karen Cote'
Between the Sea and Sky by Jaclyn Dolamore
Split Infinity by Thalia Kalkipsakis
Simple Arrangement by McKenna Jeffries
The Whites and the Blues by Dumas, Alexandre, 1802-1870
The Marines of Autumn: A Novel of the Korean War by James Brady
I Was Jane Austen's Best Friend by Cora Harrison
Nazi Germany and the Jews: The Years of Persecution, 1933-1939 by Saul Friedländer