Pediatric Primary Care (108 page)

B. Occurrence.
1. Most common cause of bow legs in toddlers.
2. Varum is greatest at 6 months of age, may progress to neutral by 18–24 months of age.
3. Adult physiologic valgus (knock knee): about 8°, typically reached by 5–6 years of age.
C. Clinical manifestations.
1. Pain-free bowing appearance to legs of toddler.
D. Physical findings.
1. Gentle curve to entire leg.
2. Normal knee flexion, extension without pain.
3. Normal progression: 15° genu varum at birth (
Figure 30–8
); 0° (straight) 18–24 months; 10–12° genu valgum (knock knees) at 30 months to 4 years; 0° (straight) to 4–6° genu valgum normal at 4–6 years.
E. Diagnostic tests.
1. Radiographic bowing of entire limb, no acute angulation seen
(
Figure 30–8
).
2. Medial proximal tibial physeal changes suggestive of pathology (Blount's disease), refer to orthopedist.
F. Differential diagnosis.
| Achondroplasia, 756.4 | Osteogenesis imperfecta, 756.51 |
| Blount's, 732.4 | Osteomyelitis, 730.2 |
| Chondrodysplasia, 756.4 | Renal failure, 593.9 |
| Leg fracture, 827 | Rickets, 268 |
1. Blount's, vitamin D-resistant rickets, renal failure, chondrodysplasia, achondroplasia, osteogenesis imperfecta, osteomyelitis, neoplasm, fracture.
G. Treatment.
1. Generally resolve spontaneously.
Figure 30–8
Physiologic genu varum. Normal “beaking” of distal femur and proximal tibial metaphysis.

Source:
Courtesy of Miki Patterson.
2. Refer to orthopedics for obvious asymmetry, clear progressive deformity, or if associated with pain.
3. Osteotomy and correction of angulation may be performed using internal or external fixation devices.
H. Follow up.
1. Return visits every 3–6 months.
I. Complications.
| Blount's, 732.4 |
| Tibia vara, 732.4 |
1. Tibial vara or Blount's disease (abrupt deformity medial proximal tibia).
2. May be seen in younger than 5 years of age but more common in adolescents.
3. Females > males.
4. Bilateral 80% of time.
5. Higher incidence in obese and African American children.
6. Will not correct with age.
J. Education.
1. Reassurance of normal finding.
2. Encourage child not to sleep or sit with legs tucked underneath; position might delay spontaneous correction.
XIII. IN-TOEING: METATARSUS ADDUCTUS
| Metatarsus abductus varus, 754.53 |
A. Etiology.
1. Unknown, theory of intrauterine position.
B. Occurrence.
1. Most common childhood foot problem.
2. 1 in 5000 births.
3. 1:20 in sibling.
4. Males, twins, preterm infants have higher incidence.
5. Seen first year of life; left > right, often bilateral.
C. Clinical manifestations.
1. Medial deviation of forefoot on hindfoot, in-toeing gait.
D. Physical findings.
1. C-shaped foot.
E. Diagnostic tests.
1. No radiographs needed for infants.
2. Children older than 4 years of age should have standing foot films, 3 views.
F. Differential diagnosis.
| Spastic anterior tibialis, 781 |
| Talipes equinovarus, 754.51 |
1. Spastic anterior tibialis.
2. Talipes equinovarus (clubbed foot).
G. Treatment.
1. Most will correct with normal use.
2. Severe deformity: Refer to orthopedist for stretching, serial casting of flexible conditions; surgical intervention is rare.
H. Follow up.
1. Per orthopedics until deformity is corrected.
2. Serial casting may be done weekly. Have parents remove semirigid cast night before appointment. Teach to stretch, then apply new cast with orthopedist holding position.
I. Complications.
1. Cast/skin complications.
2. Neurovascular problems.
3. Incorrect position, especially if cast slips and toes are no longer visible (common with infants).
J. Education.
1. Most resolve spontaneously.
2. Return to orthopedist if circulation problems, irritability (e.g., suspect cast is bothering child), or if child kicks cast off.
XIV. IN-TOEING: TIBIAL TORSION
| Tibial torsion, 736.89 |
A. Etiology.
1. Normal development in utero, genetic influence.
B. Occurrence.
1. Birth 0–20° internal tibial rotation normal: 90% correct with growth, adults achieve 0–20° of external rotation.
C. Clinical manifestations.
1. Curved appearance to tibia or in-toeing or out-toeing gait.
2. If knees are pointing forward, feet may either point in (internal tibial torsion) or out (external tibial torsion); becomes less noticeable with running.
D. Physical findings.
1. Thigh-foot angle
(
Figure 30–9
).
Child prone with knee bent at 90° angle of imaginary line drawn down thigh and middle of foot. Normal 0–30° external.
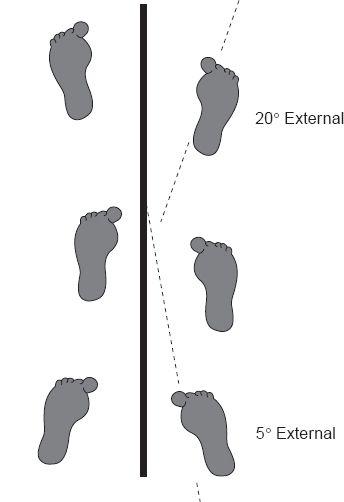
2. Foot progression angle is angle of foot compared to line extended in front of ambulating child. Best observed from directly behind patient
(
Figure 30–10
).
Figure 30–9
Thigh-foot angle. A line drawn along the axis of the femur bisects the foot.

Source:
Courtesy of Miki Patterson.
E. Diagnostic tests.
1. None if younger than 8 years of age and symmetrical pain-free appearance.
2. If needed, standing leg length X-ray (scanogram) done on long cassette.
F. Differential diagnosis.
| Hip dysplasia, 755.3 |
1. Developmental dysplasia of hip, neuromuscular conditions.
G. Treatment.
1. Observation.
2. None unless unilateral or severe or remains after age 8 years.
3. Tibial osteotomy rare but may be performed for severe cases.
H. Follow up.
1. If persists at 8 years of age, refer to orthopedist.
Figure 30–10
Foot progression angle: normal variations.
Other books
The Scene by R. M. Gilmore
Bodies and Souls by Nancy Thayer
Don't Rely on Gemini by Packer, Vin
Chosen by the Sheikh by Kim Lawrence
Lucky Bastard by S. G. Browne
Nacho Figueras Presents by Jessica Whitman
Dangerously In Love by Silver, Jordan
Kissed by Fire by Shéa MacLeod
Bicycle Mystery by Gertrude Warner
Doomwyte by Brian Jacques