Pediatric Primary Care (106 page)

Source:
Courtesy of Miki Patterson.
3. Ratio: 6 female: 1 male.
4. Left hip > right.
5. Higher frequency in firstborn children.
D. Clinical manifestations.
1. Breech birth commonly associated with this condition.
2. Difficulty diapering (abducting leg).
3. Older children may have awkward Trendelenburg gait, leg length discrepancy, pain with ambulation.
E. Physical findings.
1. Difficult in infants due to variety of levels of hip dysplasia.
2. Unequal thigh skin creases/gluteal folds.
3. Limited abduction.
4. Positive Barlow maneuver (to see if dislocatable with femur flexed and midline: adduct 10° gentle pressure posterior feel click with telescoping;
Figure 30–3
).
5. Positive Ortolani maneuver (abducting hip, feel it clunk back into place;
Figure 30–4
).
6. Galeazzi test (prone with knees flexed and heels at buttock): positive when knee heights are different
(
Figure 30–5
).
Figure 30–4
Ortolani maneuver: Abduct hip while pushing up posteriorly with fingers trying to pop hip into the socket. A click is a positive finding.
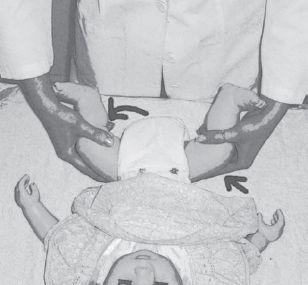
Source:
Courtesy of Miki Patterson.
Figure 30–5
Positive Galeazzi test. Note knee height difference.
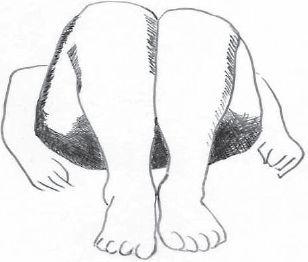
Source:
Courtesy of Miki Patterson.
F. Diagnostic tests.
| Arthrogryposis, 728.3 |
| Congenital anomalies, 759.9 |
| Leg length discrepancy, 736.81 |
| Septic hip, 711.08 |
1. Ultrasound of hips. Radiographs less helpful because femoral heads have not ossified.
G. Differential diagnosis.
1. Congenital anomalies, arthrogryposis, septic hip, leg length discrepancy.
H. Treatment.
1. Refer to orthopedist.
2. Treatment goal: Reduce femoral head to anatomic position.
3. May need Pavlik harness, hip spica cast, or surgical intervention.
I. Follow up.
1. Reexamine hips each visit.
J. Complications.
| Degenerated changes, 721.9 | Scoliosis, 737.3 |
| Dysplasia, 755.63 | Unstable gait, 781.2 |
| Low back pain, 724.2 | |
1. Delayed treatment affects normal growth of hip joint.
2. If untreated: residual dysplasia, limited range of motion, unstable gait, pain, functional scoliosis, low back pain, early degenerated changes.
K. Education.
1. Report any range-of-motion or neurovascular changes.
2. Important to hold and cuddle baby even in braces and casts.
VIII. TRANSIENT SYNOVITIS
| Fever, low-grade, 780.6 |
| Transient synovitis, 727 |
| Urinary tract infection, 599 |
A. Etiology.
1. Unknown theory of post-traumatic or allergic cause.
2. Infection frequently assumed because 32–50% follow upper respiratory tract infection.
B. Occurrence.
1. 0.2–3% of children 3–8 years of age; 6:1 male-to-female ratio.
C. Clinical manifestations.
1. Pain and limp.
D. Physical findings.
1. Symptoms present.
2. Fever absent or low grade. Do not appear severely ill.
E. Diagnostic tests.
1. Negative CBC and ESR.
2. Ultrasound positive: effusion.
F. Differential diagnosis.
| Legg-Calvé-Perthes disease, 732.1 |
| Osteomyelitis, 730.2 |
| Septic arthritis, 711 |
1. Septic arthritis
must
be ruled out. Osteomyelitis, Legg-Calvé-Perthes disease.
G. Treatment.
1. Conservative.
2. NSAIDs, rest, return to activity as tolerated.
H. Follow up.
1. If concerned, follow up in 1–2 days to be sure symptoms are resolving.
I. Complications.
| Legg-Calvé-Perthes disease, 732.1 |
| Septic arthritis, 711 |
1. Missed septic arthritis (rare).
2. 1–2% may develop Legg-Calvé-Perthes disease.
J. Education.
1. Any fever > 38.4°C or ill appearance of child should prompt reexamination.
IX. HIP PAIN: LEGG-CALVÉ-PERTHES DISEASE
| Hip pain, 719.45 |
| Legg-Calvé-Perthes disease, 732.1 |
| Transient synovitis, 727 |
A. Idiopathic AVN of femoral head in children.
B. Etiology.
1. Unknown cause of avascularity; however, multiple theories include trauma, transient synovitis, systemic abnormalities, vascular disturbances from intraosseous venous hypertension and venous obstruction.
C. Occurrence.
1. 1 in 1200 in general population.
2. 4:1 male-to-female ratio.
3. Typically 4–8 years of age.
4. Bilateral in only 15%; reported to be associated with attention-deficit/ hyperactivity disorder (ADHD).
D. Clinical manifestations.
1. Pain of groin, medial thigh, or knee.
E. Physical findings.
1. Pain with weight bearing.
2. Limited internal rotation or abduction of hip.
3. Muscle spasm may have atrophy of thigh, calf, or buttock from disuse.
4. Leg length inequality.
F. Diagnostic tests.
1. Radiographs: AP pelvis and frog lateral hips.
2. Initial X-rays may be normal; may need CT to see early changes.
3. Four stages:
a. Initial: interruption of blood supply, “crescent sign” areas of hyperand hypodense appearance of femoral head.
b. Fragmentation: epiphysis appears fragmented.
c. Reossification: normal bone density returns, deformity becomes apparent.
d. Healed: healing complete, residual deformity common.
G. Differential diagnosis.
| Knee fracture, 822 | Slipped capital femoral epiphysis (SCFE), 732.2 |
| Septic hip, 711.08 | Transient synovitis, 727 |
1. Knee problem, fracture.
2. Transient synovitis.
3. Septic hip, SCFE.
4. Neuromuscular condition.
H. Treatment.
1. Refer to orthopedist.
2. Goal: prevent femoral head deformity, alter growth disturbances.
3. Generally try to unload femoral head while allowing motion.
4. Abduction brace and bed rest, home traction with progressive abduction of legs.
5. Surgical adductor release or derotational femoral or pelvic osteotomies and spica body cast occasionally needed.
Other books
Angels Burning by Tawni O'Dell
Ice Station Zebra by Alistair MacLean
The King in Reserve by Michael Pryor
Lord Foxbridge Butts In by Manners, Robert
Tamed: A Kinky Adult Fairy Tale (Bedding the Bad Girl Book 2) by Wild, Callie
Wild Weekend by Susanna Carr
Altered Destiny by Shawna Thomas
First Kill All the Lawyers by Sarah Shankman
The Invisible Circus by Jennifer Egan
Confessions of a Call Center Gal: a novel by Lim, Lisa