Pediatric Primary Care (104 page)

b. Most important: worsening pain and tightness.
c. Compartment syndrome is accumulation of pressure in tissues, not relieved with elevation.
d. Most common areas: calves, forearms, hands, feet.
Figure 30–1
Salter I fracture. Note the increased width compared to the distal tibial physis.

Source:
Courtesy of Miki Patterson.
2. Range of motion, stretching should be pain free before beginning strengthening rehabilitation exercises then gradual return to regular activity.
II. INJURIES: FRACTURE, DISLOCATION
| Dislocation, 839.8 | Fracture, 829 |
| Ecchymosis, 459.89 | Point skin tenderness, 782 |
| Erythema, 695.9 | |
A. Etiology.
1. Damage/disruption to bone or joint, respectively, from trauma, exertion, overuse.
2. Most common causes: child abuse and neglect, sports, falls, motor vehicle or pedestrian/bicycle events.
B. Occurrence.
1. All age groups can be affected.
2. Fractures are most common presentation of child abuse; 70% of fractures in children younger than 6 months are inflicted.
3. Fractures suggestive of nonaccidental trauma in children: metaphyseal, rib (seen in 5–20% of abused children), scapular/distal clavicle/night stick (midshaft ulna), vertebral fracture or subluxation, fingers in nonambulating child, humerus (except supracondylar) in those younger than 3 years of age, bilateral/multiple fractures in different stages of healing as well as complex skull.
C. Clinical manifestations.
1. Felt tearing or heard “pop” or “crack.”
2. Most affect function.
3. Findings suspect for abuse:
a. Fracture in child younger than 1 year of age.
b. Unknown or unwitnessed injury.
c. Delay in seeking medical attention.
d. Changing story of how injury occurred.
e. Fracture does not fit mechanism described (e.g., twisting an extremity will result in spiral fracture, whereas direct blow produces transverse fracture).
D. Physical findings.
1. Pain, point tenderness, swelling, ecchymosis or erythema, loss of function, obvious deformity.
E. Diagnostic tests.
1. Radiographs in two planes: AP and lateral or both obliques.
2. May require computed tomography (CT) scan or MRI for complex injuries (i.e., pelvis or spine).
F. Differential diagnosis.
| Sprain, 848.9 |
1. Sprain.
G. Treatment.
1. Protect with immobilization/splinting, compression, ice, elevation.
2. Do not use extremity.
3. Pain medication (typically narcotic) such as acetaminophen (Tylenol) with codeine at 1 mg/kg of body weight every 4–6 hours for small children or hydrocodone (Vicodin), oxycodone (Percocet), or morphine by weight for those > 100 pounds.
4. Dislocation and displaced fractures refer stat to orthopedist. Oral medication should not be used if surgical intervention is an imminent possibility.
H. Follow up.
1. Should be per orthopedist.
2. Many will not allow use of extremity for a period of time while healing.
3. Muscles will spasm around fracture to try to pull bone ends together for healing.
4. Fractures without fixation move for 10–14 days after injury while granulation occurs (even in casts).
5. Frequent X-rays may be needed to ensure alignment of fractures.
6. In 2–6 weeks: callus develops, bone ends become “sticky,” pain is reduced.
7. Consolidation begins at 3 weeks in infants, may take 3–6 months in older children, adults.
8. Weight bearing, casting, splinting, bracing, or full use are all related to fracture configuration, healing, patient specifics.
9. Remodeling of bone that occurs in children younger than 8 years of age allows acceptance of angulated fractures.
10. Increased circulation to fractured bone causes some overgrowth (basis for 1-cm overlap of fractured femurs in young children).
I. Complications.
| Compartment syndrome, 958.8 |
| Loss of alignment, 781.2 |
| Skin abrasion, 919 |
1. Compartment syndrome.
2. Loss of alignment.
3. Shortening, angulation, delayed or nonunion of fracture.
4. Skin breakdown.
5. Neurovascular problems.
6. Infection.
7. Missed abuse.
J. Education.
1. Same as for sprains.
2. Family should seek medical attention for neurovascular changes or pain inside cast/splint/brace.
III. BACK PAIN
| Scoliosis, 737.3 |
| Back pain, 724.5 |
A. Etiology.
1. See Differential Diagnosis (below).
B. Occurrence.
1. Most common in preadolescent and adolescent.
C. Clinical manifestations.
1. Complaint of back pain, sometimes night pain (red flag), with/without numbness or tingling.
D. Physical findings.
1. May or may not have:
a. Deformity of spine.
b. Pain with motion.
c. Positive straight leg raise sign.
d. Tight hamstrings (unable to sit upright with legs extended straight out in front).
e. Neurologic changes or skin lesions.
E. Diagnostic tests.
1. Radiographs: AP and lateral thoracolumbar and/or lumbosacral spine.
2. Other testing as exam or history indicates (e.g., bone scan, MRI, labs: complete blood count (CBC) with differential, erythrocyte sedimentation rate [ESR], antinuclear antibodies [ANA], rheumatoid factor, or human leukocyte antigen B27 [HLA-B27]).
F. Differential diagnosis.
| Ankylosis spondylitis, 720 | Psoriatic arthritis, 696 |
| Degenerative disk disease, 722.6 | Reiter syndrome, 099.3 |
| Discitis, 722.9 | Scheuermann's kyphosis, 737.1 |
| Inflammatory bowel disease, 569.9 | Scoliosis, 737.3 |
| Fracture, back, 805.8 | Sickle cell crisis, 282.6 |
| Kidney infection, 590.9 | Spondylolisthesis, 756.12 |
| Menstrual cramping, 625.3 | Spondylolysis, 756.11 |
| Osteoma, 213.9 | |
1. Overuse (heavy backpacks).
Figure 30–2
(a) Spondylolisthesis (slipped forward) L-5 on S-1 with (b) spondylolysis (fractured).
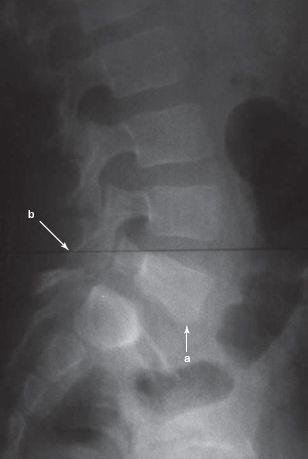
Source:
Courtesy of Miki Patterson.
2. Fracture, spondylolysis (defect or separation of pars interarticularis), and spondylolisthesis (anterior slippage of vertebral body) typically occur at L-5
(
Figure 30–2
).
3. Scheuermann's kyphosis (anterior wedging > 5° of 3 or more adjacent vertebrae).
4. Scoliosis (see later discussion).
5. Degenerative disk disease, infection, discitis.
6. Inflammatory conditions, such as ankylosis spondylitis, psoriatic arthritis, inflammatory bowel disease, Reiter's syndrome (morning stiffness is hallmark sign).
Other books
Charcoal Joe by Walter Mosley
Lucca's Lust: The Luminara Series Book 3 by SJ Molloy
Maylin's Gate (Book 3) by Matthew Ballard
Born To Be Wild by Patricia Rosemoor
Rundown by Michael Cadnum
The Believing Game by Eireann Corrigan, Eireann Corrigan
Silence Of The Hams by Jill Churchill
The Children of Urdis (Grimwold and Lethos Book 2) by Jerry Autieri
Ultimate Weapon by Ryan, Chris