Pediatric Primary Care (110 page)

2. Sling and refer to orthopedist if child fails to use arm.
H. Follow up.
1. Call or visit to ensure child is using arm normally within 1 week.
I. Complications.
1. Unreduced radius.
J. Education.
1. Teach parents mechanism of injury to prevent reoccurrence (30–40%).
XIX. GROWING PAINS
| Growing pains, 781.99 |
A. Etiology.
1. Unknown theory of periosteal irritation.
B. Occurrence.
1. Peak in 3–5 and 8–12-year olds.
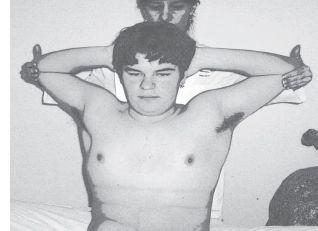
Figure 30–11
Reduction maneuver for “nursemaid's elbow.” Flex elbow to 90°, fully pronate wrist (palm down), then with gentle pressure over radial head supínate the wrist (palm up).

Source:
Courtesy of Miki Patterson.
C. Clinical manifestations.
1. Muscular pain (not joint): thighs, calves, behind knee.
2. Typically late afternoon, early evening after physically active day.
3. Can wake child from sleep.
D. Physical findings.
1. None.
E. Diagnostic tests.
1. Only if suspicious, X-ray to exclude fracture/lesion.
F. Differential diagnosis.
1. Diagnosis of exclusion:
a. No fever.
b. Not in joint.
c. No swelling, erythema, warmth.
d. No trauma.
e. No weight loss, rashes, unusual fatigue or behavior.
G. Treatment.
1. Massage, heat, acetaminophen/ibuprofen.
H. Follow up.
1. Follow up if lasts > 24 hours at time.
2. Follow up if child does not respond to medications and massage.
I. Complications.
1. None.
J. Education.
1. Normal, may come and go, child is not “faking.”
XX. COSTROCHONDRITIS
| Costochondritis, 733.6 |
A. Etiology.
1. Diagnosis of exclusion.
B. Occurrence.
1. Unknown.
C. Clinical manifestations.
1. Insidious and persistent lasting hours to days.
2. Worse with position change and deep breathing. May be diffuse or localized. Common after repetitive new activity of upper trunk and arms.
D. Physical findings.
1. Skin lesions, chest wall syndrome tests, “crowing rooster,” “horizontal arm flexion,” “hooking maneuver” diagnostic: if pain is reproduced, test is positive
(
Figure 30–12
).
2. Chest expansion test (tape measure around chest at fourth intercostal level max)–exhale then inhale = 5 cm excursion;.
E. Treatment.
1. NSAIDs, rest.
F. Diagnostic tests.
1. Radiographs of chest to rule out fracture or tumor.
2. CT, bone scan (most sensitive to rule out arthropathies, tumors, infection).
Figure 30–12
“Crowing rooster.” Elbows are pulled back and up to expand chest. A positive test is when pain is reproduced with this maneuver.
Source:
Courtesy of Miki Patterson.
3. ESR, ANA, rheumatoid factor purpose to rule out: cardiopulmonary, abdominal sources associated with rheumatologic condition or assess structure of chest wall.
G. Differential diagnosis.
| Ankylosing spondylitis, 720 |
| Fibromyalgia, 729.1 |
| Sternoclavicular hyperostosis, 733.3 |
1. Cardiopulmonary.
2. Esophagus, head, neck, and interior chest wall.
3. Ankylosing spondylitis.
4. Sternoclavicular hyperostosis.
5. Infection.
6. Fibromyalgia.
H. Follow up.
1. Within 2 weeks to document resolution of symptoms.
I. Complications.
1. Missed diagnosis.
J. Education.
1. Call for changes in symptoms.
XXI. OSTEOPOROSIS
| Osteoporosis, 733 |
A. Etiology.
1. Bony calcium deficit from various causes including lack of intake while prepubertal, absorption or metabolic origin.
B. Occurrence.
1. Disease of childhood with severe adulthood complications.
C. Clinical manifestations.
1. Majority (50–66%) of total body calcium is deposited to bone by end of puberty.
2. Earlier in females than males.
3. Highest velocity of increased bone mineral content within 9–12 months of menarche.
D. Physical findings.
1. Stress fractures, fractures with minimal trauma or no findings in childhood.
E. Diagnostic tests.
1. Lack of calcium in past 3-day diet history.
2. Poor dietary habits.
3. High suspicion in lactose-intolerant or anorectic children.
E. Differential diagnosis.
1. None.
G. Treatment.
1. Increase dietary calcium intake or supplementation.
H. Follow up.
1. Continue to assess calcium intake, stress importance to prepubertal/ pubescent children.
I. Complications.
| Dowager's hump (kyphosis), 737.1 |
| Degenerative joint changes, 721.9 |
| Fractures, 829 |
1. Fractures.
2. Dowager's hump (kyphosis).
3. Early adulthood degenerative joint changes.
J. Education.
1. Three servings of milk, cheese, yogurt daily: 1200 mg of calcium.
BIBLIOGRAPHY
American Academy of Pediatrics. Clinical practice guideline: Early detection of developmental dysplasia of the hip.
Pediatrics.
2000;105(4):896–905.
Clark MC. Approaches to child with a limp; 2003. Retrieved June 11, 2011, from:
http://www.uptodate.com/contents/approach-to-the-child-with-a-limp
.
Flynn JM, & Mehta S. An evidence-based approach to the evaluation and management of hip pain in children.
Pediatric Case Review.
2002;2(1):26–32.
Gregory PL, Biswas AC, & Batt ME. Musculoskeletal problems of the chest wall in athletes.
Sports Medicine.
2002;32(4):235–250.
Gunner KB, & Scott AC. Evaluation of a child with a limp.
Journal of Pediatric Health Care.
2001;15(1):38–40.
Hawk D & Bailie S. Pediatric/congenital disorders. In:
Core curriculum for orthopaedic nursing
Boston: Pearson Custom Publishing; 2009:259–326.
Other books
The Ironsmith by Nicholas Guild
All the Presidents' Pets by Mo Rocca
The Manchurian Candidate by Richard Condon
Green Ace by Stuart Palmer
Fierce (Storm MC #2) by Levine, Nina
Breaking the Silence by Casey Watson
The Spinster & The Coquette by Caylen McQueen
The Crescent by Deen, Jordan
Blitz Kids by Sean Longden
The Girl Next Door by Ruth Rendell