Examination Medicine: A Guide to Physician Training (77 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

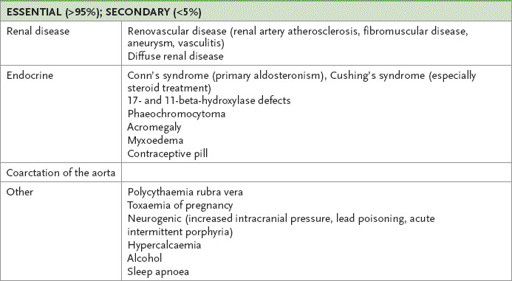
FIGURE 16.16
Chest X-ray of a patient with an ASD and right atrial and ventricular enlargement. The pulmonary arteries are very prominent (arrow). Figure reproduced courtesy of The Canberra Hospital.
a.
increased pulmonary vasculature
b.
enlarged right atrium and ventricle
c.
dilated main pulmonary artery
d.
small aortic knob.
3.
Echocardiography:
a.
paradoxical septal motion, right ventricular dilation
b.
echo dropout in atrial septum
c.
Doppler detection of a shunt at the atrial level
d.
shunt (bubble) study using agitated saline
e.
transoesophageal echocardiogram.
Indication for surgery
Almost all ASDs need to be closed surgically or if they are suitable with a percutaneous closure device when the left-to-right shunt is measured to be at least 1.5 to 1 (unless there is reversal of the shunt). A nuclear cardiac shunt study may help estimation of the shunt size.
ASD: ostium primum
This is an endocardial cushion defect adjacent to the atrioventricular valves. The signs are the same as for ostium secundum, but associated mitral regurgitation, tricuspid regurgitation or VSD is common. The ECG is particularly helpful as there is left-axis deviation and right bundle branch block (and sometimes a prolonged P–R interval). Look also for the presence of Down syndrome and skeletal upper limb defects (Holt-Oram syndrome).
VENTRICULAR SEPTAL DEFECT
The clues to the diagnosis of VSD are a thrill and a harsh pansystolic murmur confined to the left sternal edge. Sometimes mitral regurgitation is also present. Down syndrome is associated.
Results of investigations
The ECG and chest X-ray film may show left ventricular hypertrophy. The chest X-ray film may also show increased pulmonary vasculature and an enlarged right ventricle. The echocardiogram will show the defect and detect the shunt. Estimation of the pressure gradient between the ventricles will allow detection of right ventricular hypertension. As right ventricular pressure rises, the gradient across the defect falls (right ventricular pressure is closer to left ventricular) – a sign that the shunt is causing trouble.
Indication for percutaneous closure or surgery
Closure is indicated when the left-to-right shunt is moderate to large, with the pulmonary-to-systemic flow being >1.5 to 1. Often the presence of right ventricular dilatation is taken as a sign that the shunt is large.
PATENT DUCTUS ARTERIOSUS
In patent ductus arteriosus (PDA) there is a vessel from the bifurcation of the pulmonary artery to the aorta. The shunt is usually from the aorta to the pulmonary artery.
Reversal of the shunt leads to differential cyanosis and clubbing (toes,
not
fingers). Often a continuous murmur is heard. Confusion with aortic stenosis and regurgitation commonly occurs when candidates examine these patients.
Results of investigations
1.
The ECG may show left ventricular hypertrophy (diastolic overload).
2.
The chest X-ray film may show:
a.
increased pulmonary vasculature
b.
calcification of the duct (trumpet-shaped calcification)
c.
an enlarged left ventricle.
3.
Doppler echocardiography will demonstrate continuous flow in the main pulmonary artery. Left atrial size will be increased.
Indication for surgery
The indication for surgery or use of a closure device (surgery for this condition in adults is difficult and is now largely replaced by the use of percutaneous catheter closure devices) is the diagnosis of PDA with more than a trivial shunt (unless there is pulmonary hypertension).
HINT
The detection of a trivial shunt at echocardiography in a patient with a PDA but without a significant murmur or any symptoms is not an indication for closure.
COARCTATION OF THE AORTA
The most common site for this lesion is just distal to the origin of the left subclavian artery. Look for a better developed upper body, radiofemoral delay, hypertension in the arms only, chest collateral vessels, a midsystolic murmur over the praecordium and back, and changes of hypertension in the fundi. Turner’s syndrome may be associated in some cases.
Results of investigations
1.
The ECG may show left ventricular hypertrophy (systolic overload).
2.
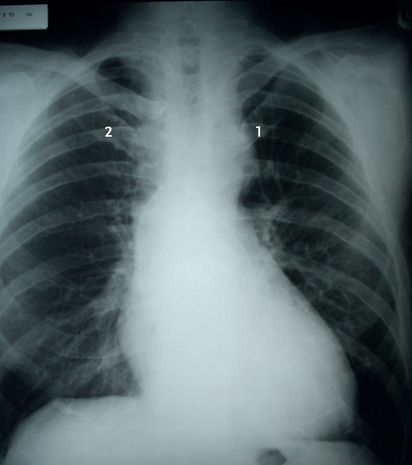
The chest X-ray film (see
Fig 16.17
) may show:
FIGURE 16.17
Chest X-ray showing coarctation of the aorta. Note the small aortic knuckle (1) and rib notching (2). Figure reproduced courtesy of The Canberra Hospital.
a.
enlarged left ventricle
b.
enlarged left subclavian artery
c.
dilated ascending aorta
d.
aortic indentation
e.
aortic prestenotic and poststenotic dilation
f.
rib notching – second to sixth ribs on the inferior border.
3.
Echocardiography may show:
a.
left ventricular hypertrophy
b.
coarctation shelf in the descending aorta
c.
abnormal flow patterns in the same area.
Cyanotic congenital heart disease
This is a very difficult area. You probably will not be expected to identify the exact lesion. A cardiac cause should be suspected if the patient shows clubbing and cyanosis.
The common causes of the problem in adults are:
1.
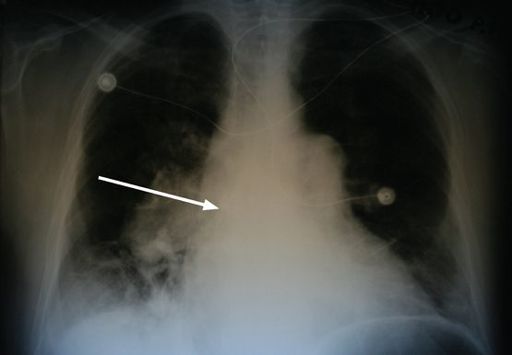
Eisenmenger’s syndrome (
Fig 16.18
) – pulmonary hypertension plus a large communication between the left and right circulations (e.g. VSD, PDA, ASD)
FIGURE 16.18
Chest X-ray of a patient with Eisenmenger’s syndrome due to an untreated VSD: the pulmonary arteries are enormous centrally (arrow) but small in the periphery. Figure reproduced courtesy of The Canberra Hospital.
2.
tetralogy of Fallot
3.
complex lesions – univentricular heart, Ebstein’s anomaly (if there is an associated atrial septal defect with a right-to-left shunt).
You must decide while examining the patient whether pulmonary hypertension is present, as this distinguishes Eisenmenger’s syndrome from the tetralogy of Fallot.
EISENMENGER’S SYNDROME
This syndrome may be found in older adults who had right-to-left shunting before the availability of open-heart surgery. The physical signs may include cyanosis, clubbing and polycythaemia. The JVP pattern may have a dominant
a
wave and sometimes a prominent
v
wave. A right ventricular heave and a palpable pulmonary component of the second heart sound (P2) may be found. On auscultation there may be a loud P2 (S2 is split and the second component is loud), a fourth heart sound, a pulmonary ejection click, pulmonary regurgitation and sometimes tricuspid regurgitation (but there may be no murmurs). The signs all add up to pulmonary hypertension in a cyanosed patient.
To work out the level of the shunt, pay close attention to the second heart sound:
1.
wide fixed split – ASD
2.
single second sound – VSD
3.
normal second sound or reversed splitting – PDA (look for differential cyanosis).
HINT
Despite traditional teaching, a loud P2 has little correlation with the presence of pulmonary hypertension, but a palpable P2 correlates well. It is said that a loud P2 is more a sign that a patient is thin than of anything else.
Results of investigations
1.
The ECG may show:
a.
right ventricular hypertrophy
b.
P
pulmonale.
2.
The chest X-ray film (see
Fig 16.18
) may show:
a.
right ventricular and right atrial enlargement
b.
pulmonary artery prominence
c.
increased hilar vascular markings but attenuated peripheral vessels
d.
a heart that is
not
boot-shaped.
3.
Echocardiography will define the anatomy and enable measurement of pulmonary pressures.
TETRALOGY OF FALLOT
There are four features:
1.
VSD
2.
right ventricular outflow obstruction (which determines severity)
3.
overriding aorta
4.
right ventricular hypertrophy.
The physical signs may include cyanosis, clubbing, polycythaemia, a right ventricular heave and a thrill at the left sternal edge, but not cardiomegaly. On auscultation there may be a single second heart sound (A2) and a short pulmonary ejection murmur.
Results of investigations
1.
The ECG may show:
a.
right ventricular hypertrophy
b.
right-axis deviation.
2.
The chest X-ray film (see
Fig 16.19
) may show:
FIGURE 16.19
Chest X-ray of a child with tetralogy of Fallot. Figure reproduced courtesy of The Canberra Hospital.
a.
a normal-sized heart with a boot shape (i.e. a left concavity where the pulmonary artery is normally situated plus a prominent elevated apex)
b.
right ventricular enlargement
c.
decreased vascularity of lung vessels
d.
right-sided aortic knob, arch and descending aorta (25%).
3.
Echocardiography will demonstrate the anatomical abnormalities.
The hypertensive examination
‘This 30-year-old man has hypertension. Please examine him.’
Method
1.
Stand back and inspect the patient. Look for evidence of Cushing’s syndrome, acromegaly, polycythaemia and uraemia (see
Table 16.6
). If one of these is present, modify your examination appropriately.
Table 16.6
Causes of hypertension