Examination Medicine: A Guide to Physician Training (37 page)
Read Examination Medicine: A Guide to Physician Training Online
Authors: Nicholas J. Talley,Simon O’connor
Tags: #Medical, #Internal Medicine, #Diagnosis

4.
In resistant ascites, an alternative is TIPS. Remember though that this is contraindicated in encephalopathic patients.
5.
Nutrition is important for these decompensated patients. Naso-gastric feeding has been shown to be helpful.
6.
Liver transplantation is the definitive treatment in suitable patients (in the absence of hepatorenal syndrome).
RENAL FAILURE AND CIRRHOSIS
Renal impairment in cirrhosis is not always due to hepatorenal syndrome (HRS), and first you must look for and cease any nephrotoxic drugs if possible (especially NSAIDs and diuretics), exclude infection (e.g. spontaneous bacterial peritonitis), ensure hypovolaemia is identified and corrected, and consider other causes of renal disease (e.g. hepatitis C or B glomerulonephritis – look for proteinuria, casts etc). Hepatorenal syndrome occurs in those with advanced chronic liver disease or liver failure and can be acute and rapidly progressive (type I) or subacute with a better prognosis (type II). The diagnosis of HRS is based on excluding the risk factors above and lack of improvement over 48 hours during volume expansion with albumin. Diuretics should have been stopped. If the diagnosis of HRS is made, a vasoconstrictor is added (a vasopressin analogue or alpha-adrenergic agonist), and listing for transplant should be considered.
HEPATITIS B
Hepatitis B virus (HBV) may be transmitted parenterally (intravenous drug users, infected blood products etc.) or sexually. Infection is common among New Zealand Maoris and people from Southeast Asia. Most infected individuals seroconvert and develop immunity; however, a small proportion become chronic carriers or progress to chronic hepatitis and ultimately cirrhosis. The risk of developing HCC in the latter group is high.
The diagnosis of hepatitis B is made by positive serology (HBsAg-positive) and active disease is usually associated with the HBeAg-positive state, as well as elevated serum transaminase levels, particularly the serum ALT level (
Table 7.13
).
Table 7.13
Interpreting hepatitis (hep) B serological testing
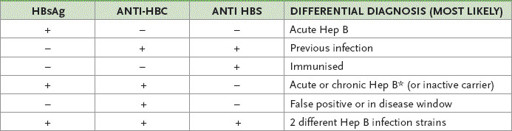
*
High ALT and AST indicates infection (versus carrier); HBC = hepatitis B core antibody; HBS = hepatitis B surface antibody
Measuring for HBV-DNA provides a more accurate assessment of viral load. Precore mutants of HBV are usually diagnosed in patients who are HBeAg-negative and HBeAb-positive, but have elevated transaminase and HBV-DNA levels.
The most accurate method of staging the disease is by means of a liver biopsy. The liver biopsy is important to assess the extent of the inflammation and fibrosis in those with chronic hepatitis.
Management
1.
The aim of antiviral therapy is to stop viral replication (i.e. seroconversion from positive HBeAg to negative HBeAg and HBV-DNA levels), as well as normalising
ALT levels and histology. ‘Inactive carriers’ (normal transaminases, HBV-DNA <10
5
copies/mL and normal biopsy) do not need antiviral therapy.
2.
Treatment is with subcutaneous peg-interferon, most commonly 5 million units thrice weekly for 2 to 6 months, or entecavir (or lamivudine) for as long as necessary. Interferon produces a response rate of approximately 30% with loss of HBeAg status and no resistance. Younger patients and women contemplating pregnancy are usually offered interferon. Nevertheless, the drug has many debilitating side-effects and is contraindicated in decompensated liver disease. Lamivudine has minimal side-effects, with a seroconversion rate after 2 years of about 30%. Lamivudine is an orally active nucleoside analogue that interferes with HBV replication, but is prescribed less often now. Long-term use of lamivudine may be associated with the development of a
YMDD
mutant form of HBV. To date these variants have not been shown to cause any additional liver damage. Patients should be maintained on lamivudine, despite the presence of the variant, because re-emergence of wild-type virus may have a worse outcome. Drug resistance to entecavir is low. Adefovir is active against lamivudine-resistant HBV.
3.
Liver transplantation can be considered in patients with decompensated HBV liver disease, but without proper preparation HBV infection recurs in the transplanted liver and may cause very aggressive liver disease. Fortunately, strategies are available to overcome this problem. Currently, antiviral drugs are used prior to transplantation to lower HBV-DNA levels and then large doses of hepatitis B immunoglobulin are used in the peritransplantation period. This strategy is extremely effective in preventing recurrence after liver transplantation.
HEPATITIS C
Hepatitis C virus (HCV) is predominantly parenterally transmitted and is particularly common in intravenous drug users. The virus is also commonly found in migrants from endemic regions, including Southeast Asia, Egypt and Italy. The majority of patients are incidentally found to be infected and are usually asymptomatic, although fatigue is a common symptom. If HCV antibody positive, confirm the diagnosis with HCV RNA.
Extrahepatic manifestations are listed in
Table 7.14
. The disease process is insidious in onset.
Table 7.14
Extrahepatic manifestations of hepatitis C

Approximately 80% of infected individuals go on to develop chronic hepatitis over a 20-year period. It is estimated that 20–30% of patients with chronic hepatitis C develop cirrhosis, but the process is generally slow and insidious. Once cirrhosis develops, symptoms are more common and the signs of end-stage liver disease can appear with jaundice, weakness, wasting and gastrointestinal bleeding. After 25 years of infection about 4% of patients with cirrhosis develop HCC.
Diagnosis is based on a positive HCV antibody ELISA test and then the active virus is checked with HCV-polymerase chain reaction (PCR) testing. Quantitative
HCV-PCR is useful in monitoring the response to treatment. A liver biopsy is helpful to stage the disease and estimate the extent of fibrosis, although the non-invasive fibroscan is replacing liver biopsy in practice. Patients with cirrhosis respond poorly to antiviral therapy and are also at risk of developing HCC.
Management
1.
Currently, therapy is prescribed for chronic hepatitis C patients with abnormal transaminases and no contraindications (e.g. uncontrolled depression). Treatment in cirrhosis is generally reserved for those who are well compensated (no ascites or encephalopathy, INR<1.5, albumin > 34 g/L, bilirubin < 26 mmol/L, platelets >75 000).
2.
Antiviral treatment is based on a combination of oral ribavirin
and
weekly injections of pegylated interferon and a protease inhibitor (boceprivir or telaprevir) (if genotype 1), or ribavirin and interferon (if genotype 2 or 3). Sustained response rates can be achieved in approximately 70% of patients with genotype I and 80% in the remainder with current regimens. Watch for depression (interferon) and haemolytic anaemia (ribavirin). Ribovarin is contraindicated in pregnancy. Do
not
treat with interferon if there is cirrhosis. There is a higher response to interferon in those with the CC variant of the
IL28B
gene.
3.
Vaccination against hepatitis A and B is recommended for patients who are not already immune.
4.
Patients who develop end-stage liver disease may be transplant candidates. Hepatitis C-related liver disease is the most common reason for liver transplantation today.
5.
Surveillance for hepatocellular carcinoma (hepatoma) is recommended if there is cirrhosis from any cause and especially hepatitis C or B. Ultrasound every 6 months is recommended; alpha fetoprotein is no longer routinely measured. Small tumours can be resected if the patient is not cirrhotic (with the best outcomes if solitary with no vascular invasion). Otherwise transplant is sometimes possible (if advanced liver disease with a solitary tumour ≤5 cm or up to three tumours all ≤3 cm) and can be curative. Palliative approaches (or as a bridge to transplant) include radiofrequency ablation (RFA) or transarterial chemoembolisation (TACE). For advanced hepatoma, sorafenib (a multitargeted tyrosine kinase inhibitor) improves survival.
HAEMOCHROMATOSIS
This is an autosomal recessive disease marked by progressive iron loading of parenchymal cells of the liver, pancreas, heart and other organs. The diagnosis is now most often made before any symptoms develop (the result of routine iron studies) and is much more common in men (menses protect women).
Symptomatic patients usually present with hepatomegaly and abdominal pain. HCC occurs in up to 30% of patients with cirrhosis. Diabetes mellitus is a classical presentation, as is grey skin pigmentation (‘bronzed diabetes’), dilated cardiomyopathy, arthropathy (second and third metacarpophalangeal (MCP) joints) and impotence (owing to iron pigmentation in the pituitary gland).
Hereditary haemochromatosis is a common genetic disorder in Caucasians, with a prevalence of at least 1 in 250. Diagnosis is suggested by an increased transferrin saturation (>62% men, >50% women) and a raised ferritin level (>300 μg/L in men and >200 μg/L in women is suggestive). The serum ferritin level is an acute-phase reactant and may be elevated in other chronic inflammatory conditions, notably those involving the liver, including non-alcoholic steatohepatitis (NASH), alcoholic liver disease and chronic viral hepatitis.
Diagnosis is made by looking for the genetic defects. In difficult cases, liver biopsy is useful to measure the amount of iron overload and the extent of liver disease (fibrosis, cirrhosis etc.). There are specific features on biopsy; a Perl’s Prussian blue stain visually demonstrates the extent of iron overload. It is important to determine the hepatic iron concentration and index (usually >1.9) on liver biopsy specimens.
The genetic defect has been localised to the short arm of chromosome 6. The gene has been termed
HFE
. Two mutations have been described:
C282Y
and
H63D
. Patients with phenotypic haemochromatosis are usually homozygous for the
C282Y
mutation; a few are compound heterozygotes (
C282Y
and
H63D
mutation). Homozygotes for
H63D
may not be at risk; 5% of those with haemochromatosis have none of these mutations. Genetic testing is recommended for all first-degree relatives of the proband.
In those cases homozygous for
C282Y
, there is a one in four chance of the siblings being homozygous. The children’s chance of developing haemochromatosis depends on the other parent (homozygous normal indicates no risk).
Management
1.
Treatment is through regular venesection (weekly) for approximately 2 years and then once every 3 months. The optimal regimen is not established, but the aim is to reduce iron stores as quickly as possible: 50 units of blood removed per year equals about 12.5 g of iron withdrawn. Patients with iron overload as a result of mutations of the iron export protein ferroportin may not tolerate this rate of removal.
2.
The avoidance of alcohol is important.
3.
Arthropathy and endocrine changes do not respond to treatment.
4.
Hepatocellular carcinoma is not prevented by venesection in patients with established cirrhosis, but life expectancy is normal in those without end-organ damage whose iron stores are reduced.
NON-ALCOHOLIC STEATOHEPATITIS (NON-ALCOHOLIC FATTY LIVER DISEASE)
Non-alcoholic steatohepatitis is defined by histological features, resembling those of alcoholic hepatitis, which are present in patients who have not consumed excessive quantities of alcohol. The majority of patients present because they are inadvertently found to have abnormal liver function tests or steatosis detected on imaging. Even though clinical findings are uncommon, hepatomegaly is the most frequent sign detected. The typical liver function abnormalities are a two- to threefold elevation of the serum aminotransferase levels, with the serum ALT greater than the serum AST level (the opposite of alcoholic liver disease). The serum gamma-glutamyl transferase (GGT) levels are also similarly elevated. Viral markers are absent.