Fundamentals of Midwifery: A Textbook for Students (105 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
13.22Mb size Format: txt, pdf, ePub
protect and improve the nation’s health and to address inequalities
’ as an executive agency of the DH (DH 2011). The Health and Social Care Act (2012) instituted health and wellbeing boards through which key stakeholders from the Health and Social Care sectors could collaborate to improve the health and wellbeing of local populations and reduce health inequalities, using community knowledge to prioritise needs and work more cooperatively (Local Government Association 2014).
Table 11.3
NICE guidelines for the care of childbearing women and babies
 Name of guideline
Name of guideline
Identifier (CG – Clinical Guideline; PH – Public Health Guideline)
Year of publication
Antenatal Care Guideline(CG62)2008Postnatal Care Guideline(CG47)2006Antenatal and Postnatal Mental Health Guideline(CG45)2007Diabetes in pregnancy: management of diabetes and its complications from pre-conception to the postnatal period(CG63)2010Quitting smoking in pregnancy and following childbirth(PH26)2010Weight management before, during and after pregnancy(PH27)2010Pregnancy and complex social factors(CG110)2010Ectopic pregnancy and miscarriage: Diagnosis and initial management in early pregnancy of ectopic pregnancy and miscarriage(CG154)2012Social and emotional wellbeing – early years(PH40)2012249
Revisiting the midwife’s role in public health
The independent Post-2010 Strategic Review of Health Inequalities 2009 ‘Fair Society, HealthyLives’ identified a ‘social gradient’ in health (p. 15), which causes people of lower social position, to experience poorer health (Marmot et al. 2010). Recommendations to reduce this social gradi- ent were to ensure that children received the ‘best start’ in life (p. 94), through strategies such as promoting:
. . . High quality maternity services, parenting programmes childcare and early years’ educa- tion to meet need across the social gradient . . .
(p. 94)Using, a strong midwifery workforce:
. . . to provide the infrastructure to support women and their partners during pregnancy, birth and early parenthood, for delivery of services that avoid unnecessary intervention, and for ensuring that those women who do, or may, require intervention are signposted at an early stage to specialist care . . .
(p. 94)The Public Health Work stream for Midwifery 2020 (Department of Health, Department of Health Safety and Social Services, Welsh Assembly Government Scottish Government 2010) made recommendations for midwives to strengthen their role in the public health agenda, as the first professional point of contact for childbearing women; they advocated a community- based practice. Midwives should be knowledgeable about the healthcare needs of the local population and work alongside social care services to identify and support women at risk and the wider family, engaging other services when necessary. The Coalition Government, WhitePaper,‘Healthy Lives, and Healthy People’(DH 2010a) reiterated the priority of improving mater- nal health in order to:
. . . give our children a better start in life, reduce infant mortality and the numbers of low birth-weight babies. . .
(p. 5)250This was criticised for failing to explain midwives’ important contribution to health promotion and early intervention, as the lead health professionals caring for pregnant women and young babies (RCM 2011). According to the International Confederation of Midwives (ICM) (2011) legally licensed midwives’ scope of professional practice includes:
’ as an executive agency of the DH (DH 2011). The Health and Social Care Act (2012) instituted health and wellbeing boards through which key stakeholders from the Health and Social Care sectors could collaborate to improve the health and wellbeing of local populations and reduce health inequalities, using community knowledge to prioritise needs and work more cooperatively (Local Government Association 2014).
Table 11.3
NICE guidelines for the care of childbearing women and babies
 Name of guideline
Name of guidelineIdentifier (CG – Clinical Guideline; PH – Public Health Guideline)
Year of publication
Antenatal Care Guideline(CG62)2008Postnatal Care Guideline(CG47)2006Antenatal and Postnatal Mental Health Guideline(CG45)2007Diabetes in pregnancy: management of diabetes and its complications from pre-conception to the postnatal period(CG63)2010Quitting smoking in pregnancy and following childbirth(PH26)2010Weight management before, during and after pregnancy(PH27)2010Pregnancy and complex social factors(CG110)2010Ectopic pregnancy and miscarriage: Diagnosis and initial management in early pregnancy of ectopic pregnancy and miscarriage(CG154)2012Social and emotional wellbeing – early years(PH40)2012249
Revisiting the midwife’s role in public health
The independent Post-2010 Strategic Review of Health Inequalities 2009 ‘Fair Society, HealthyLives’ identified a ‘social gradient’ in health (p. 15), which causes people of lower social position, to experience poorer health (Marmot et al. 2010). Recommendations to reduce this social gradi- ent were to ensure that children received the ‘best start’ in life (p. 94), through strategies such as promoting:
. . . High quality maternity services, parenting programmes childcare and early years’ educa- tion to meet need across the social gradient . . .
(p. 94)Using, a strong midwifery workforce:
. . . to provide the infrastructure to support women and their partners during pregnancy, birth and early parenthood, for delivery of services that avoid unnecessary intervention, and for ensuring that those women who do, or may, require intervention are signposted at an early stage to specialist care . . .
(p. 94)The Public Health Work stream for Midwifery 2020 (Department of Health, Department of Health Safety and Social Services, Welsh Assembly Government Scottish Government 2010) made recommendations for midwives to strengthen their role in the public health agenda, as the first professional point of contact for childbearing women; they advocated a community- based practice. Midwives should be knowledgeable about the healthcare needs of the local population and work alongside social care services to identify and support women at risk and the wider family, engaging other services when necessary. The Coalition Government, WhitePaper,‘Healthy Lives, and Healthy People’(DH 2010a) reiterated the priority of improving mater- nal health in order to:
. . . give our children a better start in life, reduce infant mortality and the numbers of low birth-weight babies. . .
(p. 5)250This was criticised for failing to explain midwives’ important contribution to health promotion and early intervention, as the lead health professionals caring for pregnant women and young babies (RCM 2011). According to the International Confederation of Midwives (ICM) (2011) legally licensed midwives’ scope of professional practice includes:
making appropriate referrals to other agencies and practitioners
taking preventative measures


health education
health counselling.The Compassion in Practice report (Commissioning Board Chief Nursing Officer and DH Chief Nursing Adviser 2012), subsequently, recognised the importance of strengthening the public health role of the midwife. DH and Public Health England (2013a,b) explicitly describe midwifery public health actions aimed at an individual, community and population level aimed at improv- ing health and wellbeing. The Maternity Matters report (DH 2007) promised women individu- alised and flexible care, led by a midwife, or the maternity team. The needs of women with complex social factors would be addressed through partnership with relevant agencies. Some contemporary maternal public health issues encountered by midwives are discussed below.
Maternal obesity
Tackling obesity has become a major focus of public health initiatives in the UK. The obese state, (body mass index [BMI] of ≥30 kg/m
2
) is linked to many negative health outcomes in childbear- ing women, when compared with women who are not obese (Lewis 2007; see Figure 11.10). Obese women are more prone to experiencing prolonged pregnancies and fetal macrosomia. These issues require greater obstetric and neonatal interventions. Infants of obese mothers are significantly more likely to experience stillbirth or neonatal death, have congenital anomalies and premature birth. Children born to mothers who gained excessive weight in pregnancy were significantly more likely to be overweight at aged three years (Oken et al. 2007), possibly pre- programming childhood obesity. Maternal malnutrition has been linked to childhood disease in later life (Hales and Barker 2001; CMACE 2010). Lifestyle change is indicated to protect and improve present and future maternal and child health.Nurses perceive weight as a sensitive issue to discuss and midwives have expressed concerns about how to communicate effectively with obese women without altering their relationship (Greener et al. 2010; Hansson et al. 2011; Mold and Forbes 2011; Schmied et al. 2011). This leads to potential avoidance of discussion of weight at antenatal booking and subsequent appoint- ments. Specialist weight management services have been developed to support pregnant women who are overweight or obese which are being widely replicated. Since 2010, in Hull and East Yorkshire, for example, women are referred to a specialist ‘
Healthy Lifestyle Midwife
’ from community midwifery care (NICE 2011; Hull Clinical Commissioning Group 2013). However, NICE (2010) places the responsibility on all maternity care practitioners to educate, inform and support women with weight management during the childbearing period. The ‘Healthy Start’ scheme offers financial support to pregnant women and mothers with children under four, who
 Healthy weight woman entering pregnancy BMI = 18.5–24.9 kg/m
Healthy weight woman entering pregnancy BMI = 18.5–24.9 kg/m
2
Obese woman entering pregnancy BMI
–
>
30 kg/m
2
Key: = increased risk of ...
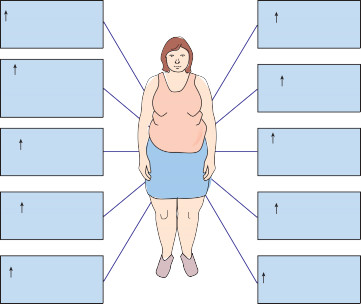
 Maternal death or severe morbiditySpontaneous first trimester and recurrent miscarriageGestational diabetesCaesarean sectionPost-caesarean wound infectionInduction of labourFailure to breastfeedHypertensive disorders including pre-eclampsiaPostpartum haemorrhageThromboembolism
Maternal death or severe morbiditySpontaneous first trimester and recurrent miscarriageGestational diabetesCaesarean sectionPost-caesarean wound infectionInduction of labourFailure to breastfeedHypertensive disorders including pre-eclampsiaPostpartum haemorrhageThromboembolism
 251
251
Figure 11.10
Additional burden of illness and complications associated with maternal obesity in pregnancy (Lewis 2007).are on low incomes, or aged under 18, to help provide them and their children a nutritious diet (Healthy Start no date). Figure 11.11 is an example of a local clinical guideline for all antenatal women, recommended by CMACE/Royal College of Obstetricians & Gynaecologists (RCOG) (2010).
Control of infectious diseases
Communicable or infectious diseases are diseases which can be transmitted from one person to another (i.e. contagious diseases) which may become endemic, epidemic or pandemic in nature (Martin 2010). Notifiable diseases must be reported to an officer of the local authority (e.g. a Consultant in Communicable Disease Control) (McCormick 1993). The virtual eradication of formerly devastating communicable diseases in the UK in the 20th century, relied upon almost universal uptake of vaccination programmes, improvements in housing and living condi- tions and a systematic and targeted public health prevention strategy, involving significant input from primary care professionals, including midwives, General Practitioners and health visitors. Indeed, the DH (2010a, p. 5) has stated that:
. . . clean air and water; enhanced nutrition and mass immunisation have consigned many killer diseases to the history books.
(DH 2010a, p. 5)IDENTIFY THE FOLLOWING
Maternal obesity
Tackling obesity has become a major focus of public health initiatives in the UK. The obese state, (body mass index [BMI] of ≥30 kg/m
2
) is linked to many negative health outcomes in childbear- ing women, when compared with women who are not obese (Lewis 2007; see Figure 11.10). Obese women are more prone to experiencing prolonged pregnancies and fetal macrosomia. These issues require greater obstetric and neonatal interventions. Infants of obese mothers are significantly more likely to experience stillbirth or neonatal death, have congenital anomalies and premature birth. Children born to mothers who gained excessive weight in pregnancy were significantly more likely to be overweight at aged three years (Oken et al. 2007), possibly pre- programming childhood obesity. Maternal malnutrition has been linked to childhood disease in later life (Hales and Barker 2001; CMACE 2010). Lifestyle change is indicated to protect and improve present and future maternal and child health.Nurses perceive weight as a sensitive issue to discuss and midwives have expressed concerns about how to communicate effectively with obese women without altering their relationship (Greener et al. 2010; Hansson et al. 2011; Mold and Forbes 2011; Schmied et al. 2011). This leads to potential avoidance of discussion of weight at antenatal booking and subsequent appoint- ments. Specialist weight management services have been developed to support pregnant women who are overweight or obese which are being widely replicated. Since 2010, in Hull and East Yorkshire, for example, women are referred to a specialist ‘
Healthy Lifestyle Midwife
’ from community midwifery care (NICE 2011; Hull Clinical Commissioning Group 2013). However, NICE (2010) places the responsibility on all maternity care practitioners to educate, inform and support women with weight management during the childbearing period. The ‘Healthy Start’ scheme offers financial support to pregnant women and mothers with children under four, who
 Healthy weight woman entering pregnancy BMI = 18.5–24.9 kg/m
Healthy weight woman entering pregnancy BMI = 18.5–24.9 kg/m2
Obese woman entering pregnancy BMI
–
>
30 kg/m
2
Key: = increased risk of ...
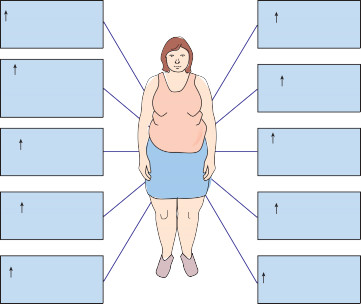
 Maternal death or severe morbiditySpontaneous first trimester and recurrent miscarriageGestational diabetesCaesarean sectionPost-caesarean wound infectionInduction of labourFailure to breastfeedHypertensive disorders including pre-eclampsiaPostpartum haemorrhageThromboembolism
Maternal death or severe morbiditySpontaneous first trimester and recurrent miscarriageGestational diabetesCaesarean sectionPost-caesarean wound infectionInduction of labourFailure to breastfeedHypertensive disorders including pre-eclampsiaPostpartum haemorrhageThromboembolism 251
251Figure 11.10
Additional burden of illness and complications associated with maternal obesity in pregnancy (Lewis 2007).are on low incomes, or aged under 18, to help provide them and their children a nutritious diet (Healthy Start no date). Figure 11.11 is an example of a local clinical guideline for all antenatal women, recommended by CMACE/Royal College of Obstetricians & Gynaecologists (RCOG) (2010).
Control of infectious diseases
Communicable or infectious diseases are diseases which can be transmitted from one person to another (i.e. contagious diseases) which may become endemic, epidemic or pandemic in nature (Martin 2010). Notifiable diseases must be reported to an officer of the local authority (e.g. a Consultant in Communicable Disease Control) (McCormick 1993). The virtual eradication of formerly devastating communicable diseases in the UK in the 20th century, relied upon almost universal uptake of vaccination programmes, improvements in housing and living condi- tions and a systematic and targeted public health prevention strategy, involving significant input from primary care professionals, including midwives, General Practitioners and health visitors. Indeed, the DH (2010a, p. 5) has stated that:
. . . clean air and water; enhanced nutrition and mass immunisation have consigned many killer diseases to the history books.
(DH 2010a, p. 5)IDENTIFY THE FOLLOWING
Height and weight to be measured not self-reported
Calculation of BMI recorded and documented in maternity hand held records and on electronic maternity records system
BMI 30 - 34.9
Book for maternity team based care.
BMI 35 - 39.9
Consultant led care should be advised to deliver in an obstetric led unit
BMI 40 - 44.9
Consultant led care, patient should be advised to deliver in an obstetric led unit. Referral to consultant anaesthetist.Women whose BMI is 40
−
44.9 will have their records reviewed by the consultant,who will then initiate a management plan documented in maternity records for antenatal care and labour. This may include requesting the women attend for an antenatal appointment with the consultant anaesthetist.
BMI 45 - and over
Consultant led care, patient should be advised to deliver in an obstetric led unit. Referral to consultant anaesthetist.Women whose BMI is 45 and over will have an antenatal appointment with the consultant anaesthetist to then initiate a management plan documented in maternity records for labour

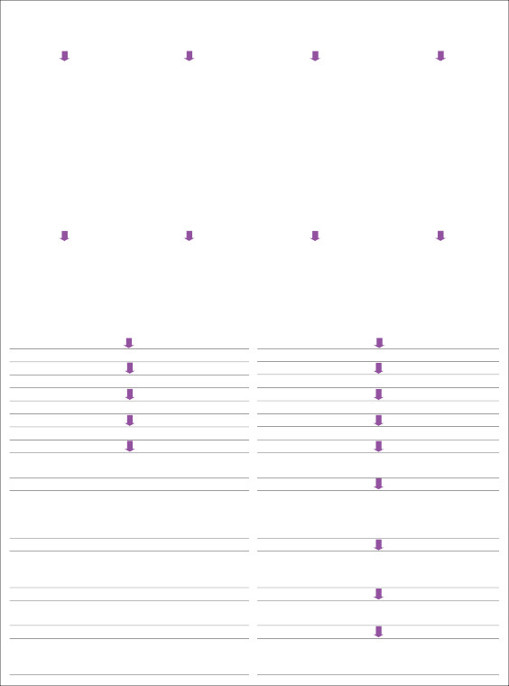 252
252
BMI 30 - 34.9
Book for maternity team based care.
BMI 35 - 39.9
Consultant led care should be advised to deliver in an obstetric led unit
BMI 40 - 44.9
Consultant led care, patient should be advised to deliver in an obstetric led unit. Referral to consultant anaesthetist.Women whose BMI is 40
−
44.9 will have their records reviewed by the consultant,who will then initiate a management plan documented in maternity records for antenatal care and labour. This may include requesting the women attend for an antenatal appointment with the consultant anaesthetist.
BMI 45 - and over
Consultant led care, patient should be advised to deliver in an obstetric led unit. Referral to consultant anaesthetist.Women whose BMI is 45 and over will have an antenatal appointment with the consultant anaesthetist to then initiate a management plan documented in maternity records for labour

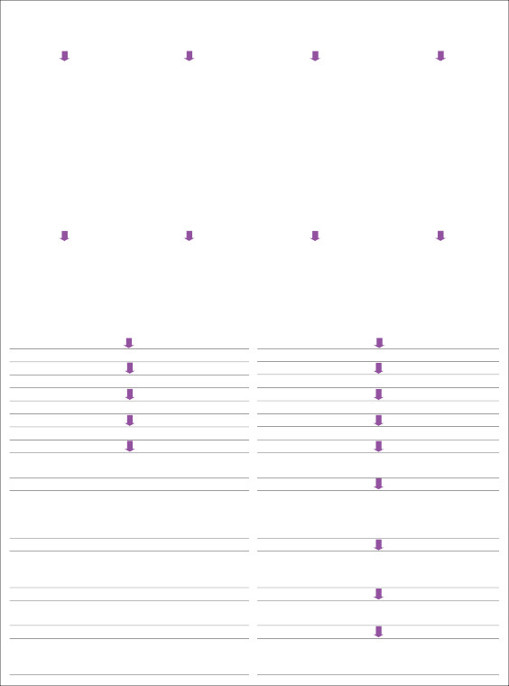 252
252Other books
Model Fantasy by Abby Gordon
The Third Coincidence by David Bishop
Frovtunes’ Kiss by Lisa Manuel
Whispers of the Dead by Simon Beckett
The Sinister Mr. Corpse by Jeff Strand
RR05 - Tender Mercies by Lauraine Snelling
The Wizards of Venus Book One: Magic Touch by Dakota Trace
For Heaven's Eyes Only by Green, Simon R.
MustLoveMusic by Jennifer Dunne
Mr. Darcy and the Secret of Becoming a Gentleman by Maria Hamilton